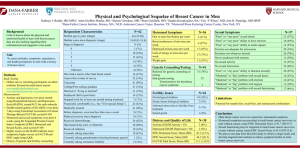
Session II: Challenging Cases
Challenging Cases from the USC Multidisciplinary
Breast Conference
Stephen F. Sener MD
Christy A. Russell MD
CS
• 41F Palpable L breast mass x 2 months
CS
•
•
•
•
•
PMH: denies
PSH: denies
Meds: denies
All: NKDA
SH: no T/E/D
• Fam Hx: sister with
breast cancer at 27,
other sister with
?uterine vs ovarian ca
• Gyn Hx:
–
–
–
–
–
–
G6 P4, miscarriage 1, abort 1
First Pregnancy: 23
Breast Feeding: 3 yrs total
Menarche: 13
Menopause: pre
OCP / HRT Hx: 10-12yrs of ocp
CS
Physical Exam
• L Breast: mod edematous
with hematoma around
core bx site at 3 o’clock,
palp mobile 2x3cm mass at
2 o’clock, and 1x1cm mass
at 3 o’clock w/ overlying
hematoma and mild ttp.
axillary LAD 1x1cm x3
• R Breast: no masses, no
nipple retraction/discharge,
no skin changes. No ax LAD
9/01/2010
9/01/2010
10/28/2010 CT CAP
Clinic Photo
Clinic Photo
CS
• MMG/UTZ (9/1/2010)
– 3.2x2.9x2.4cm mass in left
2 o’clock 4cm from nipple,
1.1cm mass at 2 o’clock
2cm from nipple. 1cm
mass at 3 o’clock 3 cm
from nipple and enlarged
LN, BR 4c
• Core Bx (9/2/2010)
– L breast: IDCA poorly
differentiated, BRS 9/9
– L axilla: c/w met IDCA
– ER-, PR– Her2: Neg
Path Photo
Path Photo
Path Photo
CS
• 41F L breast IDCA with axillary mets
– Genetics
– L MRM vs Neoadj (1071 Trial?)
CS
• Patient offered neoadjuvant chemotherapy
trial – denied
• Patient offered ACOSOG 1071 trial – agreed
• Summary: cT2, N1, M0 triple negative
multicentric infiltrating ductal breast cancer.
– Strong family history: genetic counseling
CS
• Patient received neo-adjuvant AC paclitaxel
between 10/10 and 2/11.
• Genetic testing revealed BRCA-1 deleterious
mutation.
• At completion of chemotherapy, she
underwent left MRM and right TM (3/7/11).
• Sentinel lymph node surgery performed
followed by ALND per ACOSOG 1071 trial
• Pathology: ypT2 (2.5 cm), N1 (1/31), M0
CS
• In addition to planned radiation therapy and
eventual BSO, would you offer further
adjuvant systemic therapy?
1. Yes. Change chemotherapy to include a
platinum agent
2. Yes. Change chemotherapy, but give another
regimen without a platinum agent
3. No. Watch for metastatic cancer.
CS
• Unfortunately, by May 2012, she developed a
new left supraclavicular lymph node.
• Staging workup revealed chest wall recurrence
as well as lung metastases.
• Therapy for metastatic cancer initiated.
5/12/2012 CT CAP
5/12/2012 CT CAP
Challenging Cases from the USC Multidisciplinary
Breast Conference
Stephen F. Sener MD
Christy A. Russell MD
RN
40 year old female with an erythematous
left breast x 1 month.
RN
• L Breast:
– Large palpable density in central
breast ~12cm
– Skin thickening and edema at
6:00
– 2.5cm LN palpable
• R Breast:
– No masses
– No LAD
RN on 9-12-11.
RN on 9-12-11.
RN
• PMH: none
• PSH: C-section x1
• Med: none
• FHx:
– Non-contributory
• Gynhx:
–
–
–
–
G3P3
First pregnancy at 28
Menarche 14
Premenopausal
RN
•
MMG/US 8/16/11
– RIGHT: 2:00 posterior depth 8mm cyst BR2
– LEFT: 2.9x2.3x3.1cm mass 6o’clock posterior depth BR5
– LEFT: 1.1x0.8x1.8cm mass 12o’clock posterior depth BR5
– LEFT: 1.7x0.9x1.2cm mass central anterior depth BR4C
– LEFT: 1.3x1.8x0.9cm mass 3o’clock posterior depth BR4B
– LEFT: axillary tail LN BR4B
•
Core bx 8/22/11
– LEFT: 6:00- poor diff IDCA BRS 8/9 DCIS 3/3
– LEFT: 12:00- poor diff IDCA BRS 8/9
– ER-, PR-, HER2 +
8/16/11 MMG
Extremely dense breasts
8/16/11 MMG & U/S:
3.1 x 2.9 x 2.3 cm mass in L breast @ 6:00,
BIRADS 5
1.1 x 0.8 x 1.8 cm mass in L breast @ 12:00,
1.7 x 0.9 x 1.2 cm mass in L central breast,
1.3 x 1.8 x 0.9 cm mass in L breast @ 3:00,
8 mm cyst in R breast @ 2:00,
abn LN in L axilla
8/16/11 MMG & U/S:
3.1 x 2.9 x 2.3 cm mass in L breast @ 6:00, BIRADS 5
1.1 x 0.8 x 1.8 cm mass in L breast @ 12:00, BIRADS 5
1.7 x 0.9 x 1.2 cm mass in L central breast, BIRADS 4C
1.3 x 1.8 x 0.9 cm mass in L breast @ 3:00, BIRADS 4C
8 mm cyst in R breast @ 2:00, BIRADS 2
abn LN in L axilla BIRADS 4B
RN
Pathology 1 of 4
RN
Pathology 2 of 4
RN
• 40F with multifocal L breast inflammatory CA
• Stage cT4dN1M1, ER-/PR-/Her2+.
• Staging:
– Bone scan-negative.
– CT scan of chest/abdomen/pelvis demonstrated multiple 1-3 cm
scattered pulmonary masses consistent with metastatic breast
cancer.
CTPA 10/12/2011
RN
• 40F with multifocal L breast inflammatory CA
• Stage cT4dN1M1, ER-/PR-/Her2+.
HER-2+ Inflammatory Breast Cancer
M1
• What systemic therapy would you offer this
patient?
1.
2.
3.
4.
5.
6.
Trastuzumab + taxane
Trastuzumab + capecitabine
TCH
AC TH
Trastuzumab + lapatinib
Trastuzumab + pertuzumab + docetaxel
RN
• 40F with multifocal L breast inflammatory CA
• Stage cT4dN1M1, ER-/PR-/Her2+.
• Follow-up:
– Initiated TCH x 6 in 10-11, followed by H q 3 wks
– CT scan on 6-9-2012: Marked improvement in
pulmonary metastases.
– BRCA-negative.
– Axilla cN0.
RN on 6-23-12.
Local Treatment
CTPA 10/12/2011
CT CAP 6/09/2012
IBC, HER-2+, M1
• What course of treatment would you consider
next?
1.
2.
3.
4.
Mastectomy + continue trastuzumab
Continue trastuzumab and add breast XRT
Continue trastuzumab until progression
Continue trastuzumab and add additional
chemotherapy
RN
Patient was taken to total mastectomy. She continues
on single agent trastuzumab.
SURGICAL PATH
• 6/21/12 SurgPath:
• ypT0Nx: No residual cancer, microcalcifications in benign
small ducts.
IBC, HER-2+, M1
Would you offer chest wall and extended
nodal radiation?
1. Yes
2. No
Challenging Cases from the USC Multidisciplinary
Breast Conference
Stephen F. Sener MD
Christy A. Russell MD
AG
• 39 year old female with 8 month history of
breast mass and recent severe low back pain.
• Metastases to bone only-spine, ribs, pelvis.
– posterior spinal fusion T11-L3 in 8-11.
– XRT to spine in 10-11.
• Biopsy of bone c/w breast cancer, ER/PR+,
HER-2 FISH ratio 1.8.
• Zoledronic acid from 1-12.
AG
• R Breast:
–
–
–
–
No masses
No skin changes
nipple everted
No LAD
• L Breast:
– Palpable 2cm mass @ 7:00, attached to
chest wall.
– nipple everted
– No skin changes
– No LAD
AG
AG
• PMH:
– Stage IV Breast CA s/p XRT
• PSH:
– lipoma removal x2
– 8/2011 PSF T11-L3
• Meds: leuprolide, tamoxifen,
morphine, Ca2+, oxycodone,
zoledronic acid.
•
FHx:
-
P Gma: B breast CA @ 60, esophageal CA
-
P uncle: prostate CA
-
Mother: cervical CA
•
Gyn hx:
– G4P4
– 1st child @ 16
– premenopausal
– Menarche at 13
– H/o breastfeeding
– No OCP
AG
• Patient initiated on tamoxifen and luprolide
and zoledronic acid in August 2011.
• Breast mass slowly regresses and scans
suggest no new mets and healing of bone
mets.
• Biopsy of the breast reveals residual highgrade infiltrating ductal carcinoma.
CT CAP 8/24/2011
CT CAP 11/23/2011
CT CAP 8/24/2011
CT CAP 11/23/2011
AG
-39F with L breast IDCA metastatic to bone-only,
ER+/PR+/H2N equivocal.
-Stage cT4aN0M1, Stage IV.
AG
• With ongoing clinical response to systemic
hormonal therapy and zoledronic acid,
when would you consider resection of the
primary lesion?
1. Never. No survival benefit to removing the
primary lesion
2. Now. Patient continues to have response to
original therapy
3. Later, maybe. At time of progression in the
breast.