Screening Evaluation of Spinal Pain and Disfunction
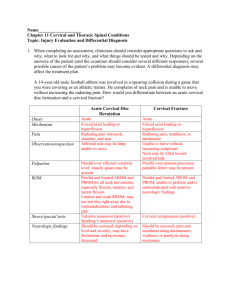
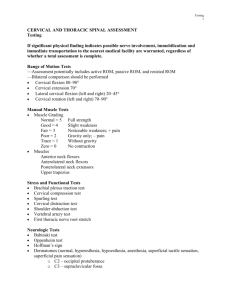
advertisement
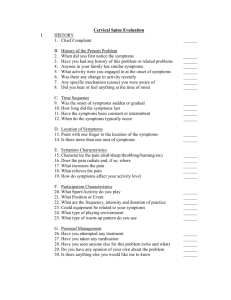
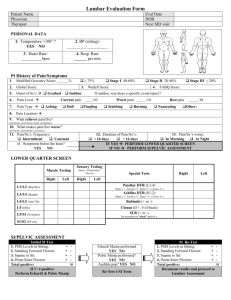
Screening Evaluation of Spinal Pain and Dysfunction John P. Kafrouni, MD Rebound Physical Medicine and Rehabilitation, Orthopedics, and Neurosurgery Scope of the Problem Low back pain/cervical pain lasting a whole day in the last 3 months – 26, 14 percent US adults. Deyo 2002 Thorasic Prevalence ranges in studies varies greatly due to study design ( 0.4 to 72%). Similar values for Lumbar/Cervical (11-84%). Briggs 2010 UNC study showed a marked rise (> double) in chronic LBP between 1992 and 2006. Possibly due to increased awareness, rising rates of depression and obesity. Among Health Care Workers District Health Care Workers in Nottingham, 1992 ½ of all respondents (n= 1363) had back pain in last year, ½ of those under age of 25 ½ of these had functionally significant pain interfering with sport, ADLs or sleep Nurses 60 % Ambulance Workers highest rates 25% had time off in last 5 years secondary to back pain Scope LBP second to URI for absenteeism in work force Cost inclusive 5,000,000 disabled due to LBP 25,000,000 Americans lose 1 or more days a year Yearly prevalence continues to grow at a rate greater than the U.S. population. RTW and Absenteeism Time Missed from Work Return to Work Expected 6 months 50% 1 year 25% 2 years 0 History is 90% - Osler (1893 or so) Temporal: - Onset abrupt, subacute, indolent - With or without apparent trauma - Improving, stable, worsening - Intermittent, AAT - Improves/worsens with activity - A.M worst? Quality: - Sharp, dull, burning, aching, nerve-like - Intensitymild/moderate/severe - 1-10 pain scale tells you more about the patient than the etiology William Osler, MD Father of Modern Clinical Training Techniques, bedside exam/history Thought one should marry a freckle faced girl. Thought clinicians older than 67 should be kindly euthanized. Provocations, Alleviation“What is the worst/best thing for your symptoms” - ProvocationsSitting Standing Walking Lifting Transitions Weight Bearing Staying Still With flexion, extension Valsalva - Alleviation Sitting Standing Walking At rest With flexion, extension Meds- may tell you a bit about the pathology, patient Categories Flexion Extension Transitional Radiation patterns are very important and underscore that often more than one thing is going on at once. Axial Radicular- true Sclerotomal- non radicular extremity pain Referable to peri- or intraarticular source Myofascial Neuropathic Red Flags Gait ataxia Sphincter dysfxn, saddle anaesthesia, ur. Retention Night pain/ weight loss Fever/chills Associated cognitive/speech/CN changes Myelopathy Myelopathy, cauda/conus injury Neoplastic Infection Upper Motor neuron Signs: consider CVA, MS, etc… The Exam Initial Observation- Seated Seated Symmetry – off loading hemipelvis- think SI joint, Hip, Ischial/trochanteric bursitis Can’t sit – Think Disc Turns torso to face you without cervical bending/rotation- think radiculopathy, cervical facet Can’t sit still- may have implications for sedentary work restrictions Posture- Seated The Exam Observation-Sit to Stand Symmetry Avoidance of specific plane Proximal muscle weakness Pain avoidance Malingering, out of proportion splinting relative to history, or simple observation of apparent distress Fear/ Anger/ Slug-like behavior Observation Posture-Standing “Take your normal comfortable posture” Asymmetry Body Parts relative to the Line of Gravity-head forward, lumbar curve, kyphosis. This gives tremendous info in myofascial pain Habitus Watch for the tendency to want to sit down, which may give an indication of general habits Posture in Standing Exam-Gait Prefers which plane? Flexion- think Spinal stenosis Antalgia Trendelenberg- weakness/pain inhibition of hip abductors. Foot drop – circumduction, hip hiking, flop/slap on heel strike. Wide based or steppage- peripheral neuropathy Spastic- myelopathy Trendelenberg Gait Initial Range of Motion: Standing Flexion Extension Lateral bending Rotation Thoracic rotation/flexion Avoidance of planes Ipsilateral or contralateral pain- joint vs. myofascial General range of motion – check cervical to compare with lumbar and vice-versa Ask specifically if back/neck and/or arm/leg pain range- assess hamstring/lumbar muscle length Thorasic Range Flexion Rotation Standing- provocation (just after/during ROM) Spurlings test Lhermitte’s test Stork test Cervical radiculopathy Cervical myelopathy Sacroiliac joint/Facet joint Confirm ipsilateral or contralateral pain and axial vs. appendicular pain- which may implicate a lateral lumbar disc Standing Provocation Spurling’s Stork Test Shoulder Screen- if no pain with cervical ROM or pure anterior shoulder pain. Posture/scapular orient Drop arm- posterior view Supraspinatus testing O’briens/AC joint Hawkins Palpation in Modified Crass position Yergeson’s or Speeds Scapular dyskinesia Painful arc Cuff Labrum Cuff Cuff- more specific Bicipital tendinosis/itis Shoulder Screen O’Brien’s Modified Crass position Palpation while standing Spinous processes Lateral masses Periscapular Myofascial Sacroiliac joint Trochanters Have the patient put a finger on “the spot” Can identify step offs with flexion/extensionspondylolisthesis Local pain Sclerotomal radiation: - Does it match claimed radiation? - Levator scapula/lateral scapula - Trochanter/IT band/PSIS medial and lateral/paraspinals/lateral sacrum. Palpation -Standing Sacroiliac joint Levator Scapula Strength while standing Heel walking Toe/heel raising Anterior tibialis- L4 predominately S-1, Gastroc/soleus Sitting Upper/Lower extremity strength/Sensation Muscle stretch reflexes Pulses Sit Slump- sensitize with ankle dorsiflexion Hip IR/ER Knee exam if indicated See myotomes/MSR Dermatomes Dural stretch- clarify axial or true radicular, myofascial, Sitting Seated Slump Dermatomes Myotomal testing Cervical C5 C6 C7 C8 T1 Delt, Biceps Pronator/Wrist Ex/Infrasp Triceps/ Ext Ind Prop Finger flex (3rd) Interossei/ Small finger abd Myotomal testing Lumbar L2 L3 L4 L5 S1 S2,3,4 Hip Flex Knee Extension Ankle dorsi, Ant Tibialis Great toe extension Toe Flexion/Heel raising Sphincter Tone Reflexes Cervical/Lumbar C5-biceps C6-pronator C7-triceps L3,4-Quads L5-Hamstrings S-1-Plantar/Gastroc soleus Pathologic reflexesHoffmans/Babinski Excessive clonus Absence of reflexesJendrassic maneuver Great range of normals, when in doubt check the upper/lower reflexes Supine evaluation Cervical pain CervicalPalpate lateral masses Greater occipital nerves Muscle tension eval Gentle traction Sclerotomal referral Repeat flexion/rotation Opportunity for muscle energy techniques Opportunity to palpate cervical structures with less muscle tension and guarding Traction may increase facet pain, decrease discogenic/radicular pain, increase or decrease muscle pain. Supine Exam Lumbar Pain Hip Scour Straight Leg Raise Sacral sheer Faber/Modified Patricks Palpate Ant/Lateral hip Faking it? SLR, Hoover’s Knee exam if indicated Flexion and Ab/Adduction Back vs. Radicular pain S.I. Joint Hip/S.I. joint Psoas /Pubic Symphysis Supine testing-Lumbar Modified Patrick’s Hoover’s sign Hoover’s sign Prone Exam Cervical and Thoracic Palpation Segmental Motion Scapular mobility Distant referral of proximal structures Palpation Costovertebral junctions Scapular mobility Opportunity for Manual Medicine techniques Prone Exam Lumbar/Pelvis Palpation -L4 is top of iliac crest Femoral stretch/Yeomans Hyper extension“up dog” Identify Spinous processes, Articular pillars Iliac Crest, PSIS, Lateral sacrum, GreatrTrochanter L2,3,4 radiculitis/SI joint Sensitizes pain of articular pillars, may decrease disc pain. Prone-Lumbar Yeoman’s Prone hyperextension Sidelying exam Gaenslens test Ober’s test FAIR test Palpation of peritrochanteric structures/ sidelying abduction Sacroiliac joint Iliotibial band Piriformis test-much talked about, seldom seen. Assessment of lateral hip syndrome. Sidelying FAIR test Ober’s test Thoughts Things that can make patients worse Anxiety Depression Fear Anger Terms like Degenerative Inactivity Narcotics, NSAIDS Perceived future disability Thoughts Treat the patient not the scan Don’t panic, call a physiatrist A bulging/herniated disc does not a surgery make, but progressive weakness, bladder/bowel changes, myelopathy, intractable pain requiring hospitalization do Thank you very much for your attention and participation Call with questions-1800 REBOUND Thank you