epidural fever
advertisement
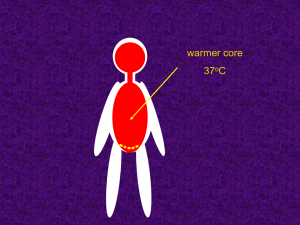
Adam Weinstein Journal Club 4/11/14 Recent attention in the literature 1:3 first time mothers develop fever (core temp >37.5 C) with CLE Maternal - Consequences: Increased HR, CO, O2 consumption Rigors, shaking Antibiotic exposure Change in obstetric plans Segal, Scott MD, MHCM. Labor Epidural Analgesia and Maternal Fever. Anesthesia & Analgesia. 2010 Dec. Vol 111.6.1467-1475 Some have even found a link to uterine rupture: - Fetal Consequences: Neonatal sepsis evaluations 3x CBC, electrolytes, LFTs, urine, CSF, imaging - Antibiotic exposure Low fetal tone Neonatal seizures Fetal hyperthermia Question of lower APGAR scores Increased neonatal encephalopathy - Meyer et al., Previc et al., Snyder-Keller et al., claim a link between autism, schizophrenia, and even Parkinson’s with maternal fever Lieberman E, Lang JM, Frigoletto F Jr, Richardson DK, Ringer SA, Cohen A. Epidural analgesia, intrapartum fever, and neo-natal sepsis evaluation. Pediatrics 1997;99:415–9 Fever is associated with decreased dopamine levels, decreased dopamine levels may stunt neonatal brain development 1.13% 1.58% 0.12% incidence in febrile mothers incidence in the acidotic fetus with neither acidosis or febrile mothers Much effort is taken to reduce acidosis: fetal monitoring, oxytocin protocols, increased rates of C-sections, drug selection NOT MUCH effort is taken to reduce a nonchorio maternal fever Impey LW, Greenwood CE, Black RS,Yeh PS, Sheil O, Doyle P. The relationship between intrapartum maternal fever and neonatal acidosis as risk factors for neonatal encephalopathy. Am J Obstet Gynecol 2008;198:49.e1–6 Goetzl L, Korte JE. Interaction between intrapartum maternal fever and fetal acidosis increases risk for neonatal Effort has not been focused on reducing fever because the mechanism remains unclear… Epidurals for C-sections and surgery result in hypothermia due to vasodilation and dissipation of heat – not increased temp However, epidurals in laboring women can result in hyperthermia 1 degree Celsius increase per 7 hours Others report 0.1 degrees Celsius per hour Segal, Scott MD, MHCM. Labor Epidural Analgesia and Maternal Fever. Anesthesia & Analgesia. 2010 Dec. Vol 111.6.1467-1475 Imbalance between heat production and dissipation, increased VO2 with contractions Opioids modestly attenuate the increase in temperature of CLE, specifically systemic IV fentanyl Maternal Inflammation: (many theories no clear answer) placental inflammation, CLE may enhance an underlying inflammatory process, spinal instrumentation Negishi C, Lenhardt R, Ozaki M, Ettinger K, Bastanmehr H, Bjorksten AR, Sessler DI. Opioids inhibit febrile responses in humans, whereas epidural analgesia does not: an explanation for hyperthermia during epidural analgesia. Anesthesiology 2001;94:218–22 Goetzl L, Evans T, Rivers J, Suresh MS, Lieberman E. Elevated maternal and fetal serum interleukin-6 levels are associated with epidural fever. Am J Obstet Gynecol 2002;187:834–8 “If intrapartum infection is one of the causes of maternal fever during epidural analgesia, then prophylactic administration of antibiotics might reduce the occurrence of such infection related fever attributed to epidural analgesia” Randomized, double blind, placebo- controlled University of Texas SW Medical Center at Dallas June 2002 – December 2005 Selected Population: Healthy nulliparous women presenting at 4-6 cm cervical dilation with contractions who requested an epidural Randomly assigned to receive either: Cefoxitin 2 grams or an identical appearing placebo – with follow up dosing 6 hours later If fever was detected: >38 C Patients were treated intravenously with: Ampicillin 2g Q6h + Gentamicin 5mg/kg Q8h Epidural Technique: 1. 500 mL bolus of LR 2. Placement of epidural catheter using a 17 gauge Tuohy needle 3. Tests dose 3 mL of 1.5% lidocaine + epinephrine 1:200,000 4. 3 mL increments of 0.25% bupivacaine titrated to a level of T10 Pelvic Exams Q2H Oxytocin augmentation if dilation <1 cm/hr Tympanic temperature measured hourly using Genius® Tympanic Thermometer Placentas were collected for histological examination Blind evaluation by a single pathologist for presence and severity of neutrophilic infiltrates - used to characterize severity of inflammation To detect a significant difference in fevers between those treated with antibiotics and those without, at least 200 patients per arm were required according to a power study of 80% where alpha = 0.05 Student t-test for normally distributed data Wilcoxon Rank Sum Test for non normal data distribution Outcome data analyzed with Breslow-Day statistic to determine differences in odds ratios 95% CI Labor characteristics and events were not statistically significant between the two arms. Within each arm 40% developed fevers and 15% required cesarean delivery. Squares represent cefoxitin group Circles represent placebo group As shown, there were no significant findings in placental characteristics between the two groups. No significant effect on any grade of neutrophillic infiltration was seen. No statistically significant differences were seen in infant outcomes: APGAR scores, cord gases, temperature at birth, birth weight, presence of meconium. Antibiotic prophylaxis did not reduce rate of fever between the two arms Antibiotic prophylaxis had no effect on any neonatal outcome Placental neutrophilic infiltration was associated with fever, but antibiotics did not reduce the fever Conclude: epidural fever cannot be attributed to maternal infection Riley et al. performed an observational study where chorion-amnion culture was not different between CLE and non CLE groups (5% vs 4%) despite a higher rate of fever among the CLE patients (23% vs 6%) This study agrees that CLE fever may not be infections in nature….. We tried to treat this fever with antibiotics… Single Center Study, Randomized, double blinded Jiaxing Maternity and Child Health Care Hospital, Jiaxing China Between 78 November 2008 and March 2009 healthy participants 78 healthy nulliparous women Singleton cephalic presentation at term Enrollment Exclusion Criteria: - Baseline temp of 37.5 C or more - Metabolic disease - Pregnancy related complications like DM/preeclampsia - Increased risk of cesarean delivery - Contraindications to CLE Epidural analgesia initiated at first request for pain relief Prior to analgesia patient data was recorded: Temperatures were recorded with a Mon-a-therm tympanic probe (thermistor YSI 400 series) Patients were randomly assigned Group I (PCEA alone) or in Group II (epidural PCEA + dexamethasone 0.2 mg/mL) PCEA: bupivacaine 0.125% and fentanyl 1ug/mL Women who delivered within two hours of analgesia or required surgical delivery were excluded Tympanic membrane temperature was measured hourly Fever was defined as at least one reading measuring 38 C or more Maternal blood at baseline, full dilatation, and cord venous blood was sampled for: IL6, TNF alpha, and IL-10 Placentas were also collected for pathological examination of the degree of Sample size of 25 patients was required at the 5% significance level (1-tailed) and a power of 90% assuming a SD of 0.6 C (P<0.05 = significance) Comparisons using independent-sample t test or Mann-Whitney U test The change in temperature over time was evaluated with repeated-measures analysis of variance Categorical variables were measured using Chi Squared or Fisher exact tests Protocol violated meaning that the patient delivered within 2 hours or had a cesarean delivery No No differences betweendifference the 2 groups with to significant inregard the mean obstetric and neonatal outcomes. No parturient had temperature atchorioamnionitis corresponding points evidence of clinical and notime neonate met was seenfor between the 2 groups, but a trend the criteria sepsis evaluation. toward elevation in the mean temperature with time was seen in group I Temperature increased by 0.4 C at 4 hours after analgesia began This mirrored an elevation in IL-6 Epidural dexamethasone reduces CLE fever and could be due to reductions in IL-6 levels IL-6 levels were not associated with clinical chorioamnionitis – indicates that infection is not responsible IL-6 could be responsible for the fever seen in CLE This finding supports that the mechanism may be due to an underlying maternal inflammatory process Epidural dexamethasone relives epidural related fever and could offer a promising prophylactic intervention Goetzl et al. showed that 100 mg of methylprednisone Q4h reduced fever by 90% but resulted in a significant increase in asymptomatic neonatal bacteremia Thomas et al. and Khafagy et al. show that epidural dexamethasone have opioid sparing, antiemetic, and antiinflammatory effects, AND reduce post epidural backache Adhesive Increased Arachadonitis Risk of Epidural abscess Hyperglycemia Risk of Meningitis So it is not for everyone: diabetics or the immunosuppressed These results are certainly interesting they may not change clinical practice today, but beg us to conduct future studies which could very well alter our standard of practice. There is a need for larger studies and furthermore dose finding studies Staff Consultant: Dr. Eli Torgeson