presentation_rocking..
advertisement

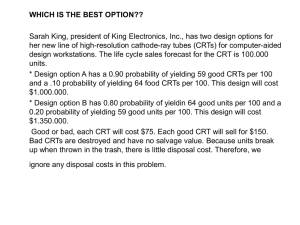
Apical Rocking and cardiomyopathy Current attempts of improving patient selection in cardiac resynchronization therapy (CRT) are mainly based on echocardiographic timing of myocardial velocity peaks. Regional myocardial function is neglected. Apical transverse motion (ATM) is a new parameter to quantify apical rocking as an integrative surrogate of both temporal and functional inhomogeneities within the left ventricle. In this study, we tested the predictive value of apical rocking for response to CRT. Methods and results Sixty-nine patients eligible for CRT were assessed by echocardiography before and 11+5 months after pacemaker implantation. Response was defined as left ventricular (LV) end-systolic volume decrease .15%. Rocking was quantified (ATM) and visually assessed by four blinded readers. Predictive value for CRT response of both assessments was compared with conventional dyssynchrony parameters. ATM in the four-chamber view plane differentiated best between responders and non-responders (2.2+1.5 vs. 0.06+1.9 mm, P , 0.0001). Quantified ATM predicted reverse remodelling with a sensitivity, specificity, and accuracy of 75, 96, and 83% whereas visual rocking assessment resulted in 89, 75, and 83%, respectively. The accuracy of conventional parameters was significantly lower. Conclusion Apical rocking is a new marker to assess LV dyssynchrony and predict CRT response. It is superior to conventional parameters. Even its simple visual assessment may be sufficiently accurate in the clinical setting. ------------------------------------------------------------------------------------------------------------------------------------ A cut-off of 1.5 mm distinguished between responders and nonresponder with a sensitivity, specificity, and accuracy of 75, 96, and 83%, respectively (Figure 2A). Contradicting reports have been published regarding the relation between a dobutamine-induced increase in either cardiac dyssynchrony or left-ventricular ejection fraction (LVEF) and the response to cardiac resynchronization therapy (CRT). Using apical rocking (ApRock) as surrogate dyssynchrony parameter, we investigated the dobutamine stress echocardiography (DSE)-induced changes in left-ventricular (LV) dyssynchrony and LVEF and their potential pathophysiological interdependence. Methods and results Fifty-eight guideline-selected CRT candidates were prospectively enrolled for low-dose DSE. Dyssynchrony was quantified by the amplitude of ApRock. An LVEF increase during stress of .5% was regarded significant. Scar burden was assessed by magnetic resonance imaging. Mean follow-up after CRT implantation was 41+13 months for the occurrence of cardiac death. ApRock during DSE predicted CRT response (AUC 0.88, 95% CI 0.77–0.99, P , 0.001) and correlated inversely with changes in EF (r 1/4 20.6, P , 0.001). Left-ventricular ejection fraction changes duringDSEwere not associated with CRT response (P 1/4 0.082). Linear regression analysis revealed an inverse association of LVEF changes during DSE with both, total scar burden (B 1/4 22.67, 95CI 23.77 to 21.56, P , 0.001) and the DSE-induced change in ApRock amplitude (B 1/4 21.23, 95% CI 21.53 to 20.94, P , 0.001). Kaplan–Meier analysis revealed that DSEinduced increase in ApRock, but not LVEF, was associated with improved long-term survival. Conclusion During low-dose DSE in CRT candidates with baseline dyssynchrony, myocardial contractile reserve predominantly results in more dyssynchrony, but less in an increase in LVEF. Dyssynchrony at baseline and its dobutamine-induced changes are predictive of both response and long-term survival following CRT. 1,5 mm !! Current imaging techniques attempt to identify responders to cardiac resynchronization therapy (CRT). However, because CRT response may depend upon several factors, it may be clinically more useful to identify patients for whom CRT would not be beneficial even under optimal conditions. We aimed to determine the negative predictive value of a composite echocardiographic index evaluating atrial-ventricular dyssynchrony (AV-DYS) and intraventricular dyssynchrony. Methods and results Subjects with standard indications for CRT underwent echo before and during the month following device implantation. AV-DYS was defined as a percentage of left ventricular (LV) filling time over the cardiac cycle. AV-DYS, which produces a characteristic rocking of the LV apex, was quantified as the percentage of the cardiac cycle over which tissue Doppler-derived displacement curves of the septal and lateral walls showed discordance. CRT responder status was determined based on the early haemodynamic response to CRT (intra-individual improvement .25% in the Doppler-derived LV dP/dt). Among 40 patients, optimal cut-points predicting CRT response were 31% for LV apical rocking and 39% for AV-DYS. The presence of either apical rocking .31% or AV-DYS ≤39% had a sensitivity of 95%, specificity of 80%, positive predictive value of 83%, and a negative predictive value of 94% for CRT response. Conclusion After pre-selection of candidates for CRT by QRS duration, application of a simple composite echocardiographic index may exclude patients who would be non-responders to CRT and thus improve the global rate of therapy Normal apical kinetics % de temps en opposition Cutt of à 31% du RR %Avdys temps diastolique/RR *100 % Ap rocking>31% % Av dys <36%