Stephanie Fanale
Brenda Wilson, Ph.D, CCC-SLP
Eastern Illinois University
Research supported by an undergraduate research grant at Eastern Illinois University
Traumatic brain injury (TBI) affects the lives of
approximately 1.7 million Americans each year (Faul, Xu,
Wald, & Coronado, 2010)
Patients with TBI often present with symptoms of impaired
awareness in regard to their injuries as well as the impact of
their injuries on their daily functioning (Sherer, Bergloff,
Boake, High, & Levin, 1998)
Due to the individualized nature of awareness, developing a
general, yet adequate assessment tool of awareness has
proven difficult
There is limited information available about the validity of
most assessments, as well as the rehabilitation implications
of awareness of deficits in people with TBI
Roberts et al. (2006) found that individuals who
received a one-on-one neurological consultation
increased their levels of self-awareness
Proctor, Wilson, Sanchez, and Wesley (2000)
found a direct relationship between having the
skills required to complete functional tasks
successfully and the ability to set realistic goals
Proctor et al. (2000) also found a direct
relationship between having the skills required
to complete functional tasks successfully and the
awareness required to self-monitor behavior
The
purpose of this study was to
determine the relationship between two
awareness measures and a functional
measure of communication.
What
is the relationship between awareness
of deficit scores and functional
communication outcome scores after TBI?
Does
severity of the brain injury impact the
relationship between awareness of deficit
scores and functional outcome scores after
TBI?
What
are speech-language pathologists’
clinical preferences in regard to awareness
assessments?
Subject #
Sex
Age of
Injury
Age at
Testing
1
Male
17:4
18:0
Left temporoparietal
laceration, intraparenchymal
hemorrhage, depressed skull
fracture, Loss of
consciousness
2
Male
17:10
17:10
Intraventricular hemorrhage/
lateral ventricles, small
hemorrhages, anterior corpus
callosum and cerebellum
3
Female
15:0
15:0
Subdural hematoma, right
parietal subarachnoid
hematoma, Loss of
consciousness
Mean age of injury = 16;9
Mean age of testing = 16;11
SD = 1.51
SD = 1.69
Description of Injury
2
awareness assessments were given:
• Awareness Questionnaire
• Functional Assessment of Verbal and Executive
Strategies (FAVRES)
Composed
of three forms: a patient form, a
significant other form, and a clinician form
On
each form, the abilities of the person with
TBI to perform various tasks after the injury
as compared to before the injury are rated on
a five point scale ranging from "much worse"
to "much better”
Awareness
of deficits is determined by
subtracting the significant other’s score and
the clinician score from the self-rating of the
participant, resulting in a discrepancy score
A standardized test designed to measure the use of
executive strategies to complete tasks specifically for those
individuals 18 or older with acquired brain injuries.
Consists of four tasks made to replicate everyday cognitive
demands. The current study measured awareness of deficits
using the rationale score for two tasks:
• Task One: “Planning an Event”—requires the participant to
analyze several options presented in a newspaper listing and
choose which event was most appropriate within the
constraints of time, money, and appropriateness.
• Task Two: “Scheduling”—requires the participant to analyze a
“things to do” list and various telephone messages in order to
organize and prioritize activities based on importance and
time.
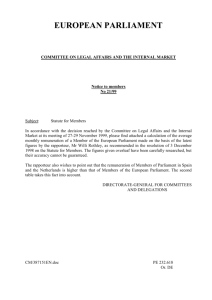
EXPRESSION
SOCIAL INTERACTION
No Helper
7: Complete Independence
6: Modified Independence
No Helper
7: Complete Independence
6: Modified Independence
Helper
5: Standby Prompting
4: Minimal Prompting
3: Moderate Prompting
2: Maximal Prompting
1: Total Assistance
Helper
5: Supervision
4: Minimal Direction
3: Moderate Direction
2: Maximal Direction
1: Total Assistance
There
was a tendency for increased
awareness of deficit, as measured by the
AQ discrepancy scores, to be associated
with a lower communication outcomes, as
measured by the FIM.
Participant 1:
• FIM score: 6 out of 14
• Lowest AQ discrepancy score: 5
Mean
FIM
8
AQ
-12
Standard Deviation
1.73
-8.89
Minimum Value
6
-5
Maximum Value
9
-22
Combined FIM & AQ Discrepancy Scores
14
12
10
8
5
9
22
6
4
2
0
0
5
10
15
20
25
There
was a tendency for increase
awareness of deficits, as measured by the
FAVRES rationale score, to be associated
with a higher communication outcome, as
measured by the FIM.
Participant 1:
• FIM score: 6 out of 14
• FAVRES rationale score: 4
Mean
FIM
8
FAVRES rationale
5.67
Standard Deviation
1.73
2.89
Minimum Value
6
4
Maximum Value
9
9
FAVRES Rationale scores & FIM ratings
14
12
10
8
4
4
8
6
4
2
0
0
2
4
6
8
10
Physical
limitations were included on the
AQ
Participant
1 was injured last summer.
Other participants were tested directly
after discharge.
FIM
ratings were used to measure severity
of injury, with lower ratings indicating
increased severity
Participant
1:
• Lowest FIM score—indicating greatest severity
• Lowest AQ discrepancy score—indicating highest
awareness
• Lowest FAVRES rationale score—indicating lowest
awareness
Combined FIM & AQ discrepancy scores
25
20
15
10
5
0
6
9
9
Combined FIM & FAVRES Rationale Score
200
150
100
50
0
6
9
9
Area
AQ
FAVRES
Ease of Administration
5
5
Time Efficiency
5
3
Accuracy of Assessing
Awareness
5
2
Based on the clinical preferences rating of the clinician, the AQ was ranked
the better than the FAVRES for time efficiency and for accuracy. Both
assessments were given the highest ratings for ease of administration .
The
AQ was the most accurate
assessment of awareness of deficit.
Awareness
of deficit as measured by the
AQ does not show a strong relationship
with the FIM expression and social
interaction scales.
The
rationale score of the FAVRES was not
an accurate assessment of awareness of
deficit
The
rationale score of the FAVRES was
moderately related to communication
outcome as measured by the FIM
In
this small sample, increased severity as
measured by the FIM was not associated
with increased awareness of deficit.
However, it was associated with the FAVRES
rationale score.
Increased
sample size will increase
validity of results.
Since
awareness of deficit is an important
factor in rehabilitation after TBI, various
measures of awareness should be
evaluation in terms of rehabilitation
outcome.
Faul, M., Xu, L., Wald, M. M., & Coronado, V. G. (2010, March 17).
Traumatic Brain Injuries in the United States. Retrieved from
http://www.cdc.gov/TraumaticBrainInjury/statistics.html
Proctor, A., Wilson, B., Sanchez, C., and Wesley, E. (2000).
Executive function and verbal working memory in
adolescents with closed head injury (CHI). Brain Injury, 14(7),
633-647. doi:10.1080/02699050050043999
Roberts, C. B., Rafal, R., & Coetzer, B. R. (2006). Feedback of
brain-imaging findings: Efects on impaired awareness and
mood in acquired brain injury. Brain Injury, 20(5), 485-497. doi:
10.1080/02699050600664665
Sherer, M., Bergloff, P., Boake, C., High, W., & Levin, E. (1998).
The Awareness Questionnaire: Factor structure and internal
consistency. Brain Injury, 12(1), 63-68. doi:
10.1080/026990598122863