Glycogen Metabolism by Dr Tarek File
advertisement

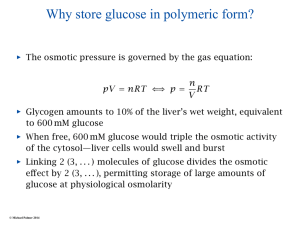
Qassim University College of Medicine Glycogen Metabolism Dr. Tarek A Salem Biochemistry Objectives • List the steps of glycogen biosynthesis (glycogenesis) • Mention site of occurrence, regulation and importance of glycogenesis. • Differentiate between liver and muscle glycogen • List the steps of glycogenolysis • Mention site of occurrence, regulation and importance of glycogenolysis. • Explain the biochemical basis of glycogen storage disorders Liver Cell Glycogen • Glycogen is the main storage form of carbohydrates in animals. It is present mainly in liver and muscle. • In the liver, glycogen can compose up to 8% of the fresh weight (100–120 g in an adult) soon after a meal. Only the glycogen stored in the liver can be made accessible to other organs. • In the muscles , glycogen is found in a much lower concentration (1% to 2% of the muscle mass), but the total amount exceeds that in the liver . Glycogen is a polymer of glucose residues linked by alpha(14) glycosidic bonds, mainly alpha(16) glycosidic bonds, at branch points. - Glycogen branches contain about 8 -12 glucose residues. Glycogenesis • It is the formation of glycogen in muscle and liver • Its site in the cytoplasm of every cells mainly liver and muscle Glycogen synthesis Steps Glucokinase 1- Glucose Phosphoglucomutase G6P G1P Mg++ ATP ADP UDP-Glucose pyrophosphorylase 2- G-1-P UDP-glucose UTP PPi H2O Pyrophosphatase 2Pi Glycogen synthesis 1-Glycogen synthase enzyme in presence of preexisting glycogen primer (glycogenin). 2- Chain is lenthened, branching enzyme transfers a part of the α-1:6 glycosidic link. 3- The branches grow up by further addition of 1:4 glucosyl units. 4- The key regulatory enzyme is glycogen synthase which present in 2 forms: - Active (dephosphorylated form) - Inactive (phosphorylated form) Glycogen synthase It catalyzes transfer of the glucose moiety of UDPglucose to the hydroxyl at C4 of the terminal residue of a glycogen chain to form an a(1 4) glycosidic linkage: Glycogen(n) + UDP-glucose Glycogen(n +1) + UDP Glycogenolysis • It is the breakdown of glycogen into glucose in liver and lactic acid in muscles. Glycogen Phosphorylase catalyzes phosphorolytic cleavage of the α(14) glycosidic linkages of glycogen, releasing glucose-1phosphate as reaction product. Glycogen(n) + Pi Glycogen (n–1) + glucose-1-phosphate CH 2OH H O H OH H H OH OH H OPO32 glucose-1-phosphate Glycogenolysis • G-1-P is converted into G-6-P by the action of phosphoglucomutase. • In liver, G-6-P is hydrolysed by the action of G-6-phosphatase free glucose • In muscle, G-6-P by glycolysis lactic acid because absence of G-6-phosphatase Pyridoxal phosphate (PLP), a derivative of vitamin B6, serves as prosthetic group for Glycogen Phosphorylase. H O O P O O C H2 C OH O N H CH3 pyridoxal phosphate (PLP) Glycogenolysis The key regulatory enzyme is glycogen breakdown which present in 2 forms: - Active (Phosphorylated form) - Inactive (Dephosphorylated form) = Debranching enzyme is hydrolytic enzyme acts on α1 6 glycosidic link giving free glucose. = Muscle glycogen is to provide muscle with glucose. = Liver glycogen is to maintain blood glucose between meals. = After 12 -18 hr fasting, liver glycogen whereas muscle glycogen is after prolonged exercise. Difference between muscle and liver glycogen Liver glycogen Muscle glycogen Amount Source Hydrolysis More in concentration Glucose and other precursore Give blood glucose More in amount Glucose only Give lactic acid Starvation Muscular exercise Converted into blood glucose Depleted Not affected Depleted Effect of Hormons Insulin Adrenaline Thyroxine Glucagon Insulin Adrenalin Thyroxine Glucagon Regulation of glycogen metabolism In Fasting: Glucagon • cAMP activates Protein Kinase A which phosphorylates and inactivates glycogen synthase • Little glycogen synthesis during fasting Regulation of glycogen metabolism In Fasting: Glucagon • cAMP activates Protein Kinase A which phosphorylates and activates glycogen phosphorylase • Fasting results in increased glycogenolysis Regulation of glycogen metabolism • In Feeding: Insulin cAMP is reduceded stimulates phosphodiesterase induces and activates protein phosphatase-1 Activates Glycogen Synthase (Glycogenesis is activated) While Glycogen Phosphorylase is inactivated (Glycogenolysis is inactivated) • Feeding results in glycogen synthesis Coordinated regulation of glycogen metabolism Glycogen storage diseases (GSD) • They are the result of defects in the processing of glycogen synthesis or breakdown within muscles, liver, and other cell types. • GSD has two classes of cause: genetic and acquired. • Genetic GSD is caused by any inborn error of metabolism. • In livestock, acquired GSD is caused by intoxication with the some alkaloids. Types of GSD • There are eleven distinct diseases that are commonly considered to be glycogen storage diseases. • Although glycogen synthase deficiency does not result in storage of extra glycogen in the liver, it is often classified with the GSDs as type 0 because it is another defect of glycogen storage and can cause similar problems.) glycogen Glycogen Storage Diseases are genetic enzyme deficiencies associated with glucose-1-P excessive glycogen Glucose-6-Phosphatase accumulation within cells. glucose-6-P Some enzymes whose deficiency leads to glycogen accumulation are part of the inter-connected pathways shown here. glucose + Pi fructose-6-P Phosphofructokinase fructose-1,6-bisP Glycolysis continued Symptoms in addition to excess glycogen storage: When a genetic defect affects mainly an isoform of an enzyme expressed in liver, a common symptom is hypoglycemia, relating to impaired mobilization of glucose for release to the blood during fasting. When the defect is in muscle tissue, weakness & difficulty with exercise result from inability to increase glucose entry into Glycolysis during exercise. Additional symptoms depend on the particular enzyme that is deficient. Glycogen Storage Disease Symptoms, in addition to glycogen accumulation Type I, liver deficiency of Glucose-6-phosphatase (von Gierke's disease) hypoglycemia (low blood glucose) when fasting, liver enlargement. Type IV, deficiency of branching enzyme in various organs, including liver (Andersen's disease) liver dysfunction and early death. Type V, muscle deficiency of Glycogen Phosphorylase (McArdle's disease) muscle cramps with exercise. Type VII, muscle deficiency of Phosphofructokinase. inability to exercise.