EEA018-lecture
advertisement

Chapter 14 Electrical Safety
References:
1. Walter H. Olson, “Chapter 14: Electrical Safety,” in J. G. Webster (ed.),
Medical Instrumentation: Application and Design, 3rd ed.. New York,
Wiley, 1998, pp. 623658.
2. David Prutchi and Michael Norris, “Design of safe medical device prototypes,” in Design and Development
of Medical Electronic Instrumentation: A Practical Perspective of the Design, Construction, and Test of
Medical Devices. New York: Wiley, 2005, pp. 97146.
The environment
Patients are exposed to more hazards in medical environments
than the typical home or workplace
Statistic
10,000 device-related patient injuries per year in the US
Reason:
Improper use of devices
Inadequate training & lack of experience
Increased complexity of medical devices
Utilization of medical devices in more procedures
User manuals are seldom read
Design
Name one device that will never go wrong.
Fail-safe design: Because all devices eventually fail.
Safe design + safe use
Concept: Everything that can go wrong will eventually go wrong.
Hazards
hazard 危險; 危害物; 危險之源
• Sources of hazards:
fire, air, earth, water,
chemicals, drugs, microorganisms,
Vermin, waste, sound,
vermin 害蟲(指鼠、蝨等); 寄生蟲
electricity, natural and unnatural disasters, surroundings,
gravity, mechanical stress, people responsible for acts of
omission and commission,
radiation from x rays, ultrasound, magnets,
ultraviolet light, microwaves, and lasers.
disaster災難
Action
* Electrically isolated patient connections of the medical equipment
* Education on safety for medical personnel
* Medical-equipment testing procedures
This chapter
• Contents:
physiological effects of electric current
shock hazard
methods of protection
electrical-safety standards
electrical-safety testing procedures.
• objectives:
to understand the possible hazards;
to incorporate safety features
into the medical instrument design
14.1 Physiological effects of electricity
Electrical current through biological tissue:
(1) Stimulation of excitable tissue
(2) Resistive heating
(3) Electrochemical burns and tissue damage (DC)
Various levels of physiological effects
Perception:
Exciting nerve endings in the skin
A tingling sensation
AC 60 Hz: threshold = 0.5 mA (moistened hands);
DC: threshold = 2-10 mA, slight warming of the skin;
Let-go:
Vigorous stimulation of nerves and muscles
Pain and fatigue
Involuntary muscular contractions
Reflex withdrawals
Let go current ≡the max current for voluntary withdrawal
The minimal threshold for the let go current = 6 mA
Various levels of physiological effects (cont.)
Respiratory paralysis, pain, and fatigue:
Involuntary contraction of respiratory muscles
(1) Asphyxiation 窒息
Respiratory arrest: 18-22 mA
(2) Pain and fatigue
Various levels of physiological effects (cont.)
VF:
The normal propagation of action potential is disrupted
Major cause of death due to electric shock
1000 deaths per year in the USA
Threshold for VF = 75-400 mA
Doesn’t stop until defibrillator is used
(Defibrillation: A brief high-current pulse depolarizes all the myocardial cells
simultaneously.)
Sustained myocardial contraction:
A normal rhythm ensues after removing the current
Threshold = 1-6 A
Burns:
Usually on the skin at the entry points
Physical injury:
Can puncture the skin if V > 240 V
Brain and nervous tissue will lose excitability when high currents pass through
them
Muscular contraction can be strong enough to pull the muscle attachment away
from the bone.
Let go current:
You = 100 mA
Your friend = 10 mA
If the current = 20 mA
Can you escape?
Can your friend escape?
Figure 14.1 Physiological effects of electricity Threshold or estimated mean values are given for each effect in a 70 kg human for a 1 to 3 s
exposure to 60 Hz current applied via copper wires grasped by the hands.
14.2 Important Susceptibility Parameters
Susceptibility易受影響姓
(1) Current magnitude
Figure 14.2 Distrubutions of perception thresholds and let-go currents These data depend on surface area of contact (moistened hand grasping
AWG No. 8 copper wire). (Replotted from C. F. Dalziel, "Electric Shock," Advances in Biomedical Engineering, edited by J. H. U. Brown and J. F.
Dickson IIII, 1973, 3, 223-248.)
(2) Frequency
Figure 14.3 Let-go current versus frequency Percentile values indicate variability of let-go current among individuals. Let-go currents for
women are about two-thirds the values for men. (Reproduced, with permission, from C. F. Dalziel, "Electric Shock," Advances in Biomedical
Engineering, edited by J. H. U. Brown and J. F. Dickson IIII, 1973, 3, 223-248.)
(3) Duration
Figure 14.4 Fibrillation current versus shock duration. Thresholds for ventricular fibrillation in animals for 60 Hz ac current. Duration of
current (0.2 to 5 s) and weight of animal body were varied. (From L. A. Geddes, IEEE Trans. Biomed. Eng., 1973, 20, 465-468. Copyright 1973
by the Institute of Electrical and Electronics Engineers. Reproduced with permission.)
Electrical devices include any weapons that use the effects of electricity to incapacitate
(使無能力) the target. There are a variety of different devices but their principle of
operation is the same. They are battery powered and use a low current, high voltage
impulse shock for incapacitation. Other terms for these devices include
Conducted Energy Device (CED)
Electro-Muscular Disruption (EMD) Device
Human Electro-Muscular Incapacitation (HEMI) Device.
Source: http://www.nldt.org/terms_all.php
Strength-duration curve
I
Id
1 e d /
Strength-duration equation
Strength- durationequation :
T hestimulation current threshold(for short durations)
I
Id
1 e d /
I : Rheobase current
: Chronaxietimeconst ant
rhe(o)- word element [Gr.], electric current; flow (as of fluids).
Rheobase 基本電位,(引起刺激之最低電位).
Chronaxie 時值,(引起肌肉收縮最少所需之電流時間).
Rheobase: theminimumnerveimpulse required to elicit a responsefroma tissue
Chronaxie(chronaxy): theminimumintervalof timenecessaryt o electrically st imulat e
a muscle or nervefiber, using twice theminimumcurrentneeded
toelicit a thresholdresponse.
(Source : http: //www.t hefreedict ionary.com/)
incapacitate 使無能力
Stimulation threshold:
= 3.5 uC/cm2 of charge transfer density
(large amplitude, < 100 us, directly to the heart)
Fibrillation stimulation threshold : single-beat stimulation threshold
= 20:1 ~ 30:1 (electrode on the heart)
= 10:1 ~ 15:1 (electrodes on the chest)
(4) Points of entry
Current threshold for VF:
LA-RA > LL-RA or LL-LA
Two points on the same hands > Two points on two hands
(4) Points of entry (cont.)
Figure 14.5 Effect of entry points on current distribution (a) Macroshock, externally applied current spreads throughout the body. (b)
Microshock, all the current applied through an intracardiac catheter flows through the heart. (From F. J. Weibell, "Electrical Safety in the
Hospital," Annals of Biomedical Engineering, 1974, 2, 126-148.)
Current threshold for microshock (of dogs): 20 μA (total current)
Current threshold for microshock (of human): 80-600 μA (total current)
Safety limit to prevent microshock: 10 μA
(5) Body weight
Threshold: increases with body weight
Threshold: increases with body weight
14.3 Distribution of Electric Power
Electric power in health-care facilities for:
Medical instruments, lighting, maintenance appliances, patient conveniences
(TV, hair curler, and electric toothbrushes), clocks, nurse call buttons, etc.
240 V for heavy-duty devices:
Air conditioner, electric dryers, x-ray machines
This section:
Safe distribution of power
in health-care facilities
Electric-power distribution
Figure 14.8 Simplified electric-power distribution for 115 V circuits. Power frequency is 60 Hz.
NEC (National Electric Code) 1996, 2006
* All receptacles be grounded by a separate insulated (green)
copper conductor (Article 517-13)
* The maximal potentials permitted between any two exposed
conductive surfaces in the vicinity of the patient (Article 517-15)
<1> General-care areas – 500 mV
<2> Critical-care areas – 40 mV
receptacle (電源)插座
Critical-care areas
•< 40 mV (Article 517-15)
•Patients are intentionally exposed to electric devices
•Single patient-grounding point
•Periodical testing of ground continuity
•Receptacles: > 6 single or 3 duplex
Unsafe
General-care areas
•< 500 mV
•Receptacles: > 4 single > 4 duplex
•Each rceptacle must be grounded
•Patients are incidentally exposed to electric devices
Ground faults
Ground fault
A short circuit between the hot conductor and ground
that injects large currents into the grounding system
ground fault
ground fault
The circuit breaker
will open due to
ground fault
Isolated power systems
In isolated power systems,
large currents into the grounding system
* will occur when there are double ground faults
* will not occur when there is a single ground fault
Isolated power systems are used in applications where
loss of power supply cannot be tolerated.
NEC requirement: isolated-power systems in operating rooms and locations where flammable anesthetics are used or
stored
Isolated power systems
C = 0.3 F, Zc = 8.8 k @60 Hz
C = 0.01 F, Zc = 26.5 k @60 Hz
Line-isolation monitor (dynamic ground detector): to detect the occurrence of the first fault from either conductor to ground
“Isolation” transformer: means to isolate the two conductors from ground
Isolated power systems
Figure 14.7 Power-isolation-transformer system with a line-isolation monitor to detect ground faults.
Emergency power systems
Article 517, NEC (1990, 2006)
The emergency electric system for health-care facilities:
Requirement automatically restoring power within 10
s after interruption
14.4 Macroshock Hazards
Skin resistance
Susceptibility to VF ? ?
Skin resistance:
Dry:
15 k-1 M/cm2
Wet or broken: 1%
Internal resistance:
chassis 底盤, 底座
Figure 14.10 Macroshock due to a ground fault from hot line to equipment cases for (a) ungrounded cases and (b) grounded chassis.
14.4 Macroshock Hazards (cont)
Possible causes:
* Failures of insulation
* Shorted components
* Mechanical failures
* Strain and abuse of power cords, plugs, and receptacles
* Spilling of fluids (blood, urine, intravenous solutions, baby
formulas)
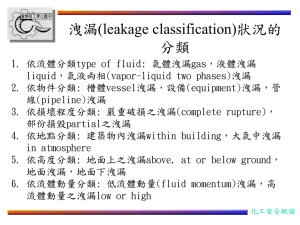
14.5 Microshock Hazards
When there are direct electric connections to the patient’s heart
Causes:
(1)Leakage current in line-operated equipment
(2)Potential difference between grounded conductive surfaces
Direct electric connections to the patient’s heart
Microshock-susceptible situations:
1.
Epicardial/endocardial electrodes of externalized temporary cardiac pacemakers
2.
Electrodes for introcardiac electrogram measuring /stimulation devices
3.
Liquid-filled catheters placed in the heart to measure blood pressure, withdraw blood samples,
inject substances such as dye or drugs into the heart, etc. (Internal R of catheter = 50 k to 1 M,
much higher than the two cases above)
It only requires a leakage current
It doesn’t require a ground fault
to induce a microshock.
(b) With a grounded electric connection to the
heart, the patient may receive a microshock
while touching the chassis whose ground wire is
broken.
(c) There is a connection from the chassis to the
patient’s heart. There is also a connection to
ground anywhere on the body. The broken
ground of the chassis could cause a microshock.
Figure 14.11 Leakage-current pathways Assume 100 µA of leakage current from the power line to the instrument chassis. (a) Intact ground, and 99.8 µA flows through the
ground. (b) Broken ground, and 100 µA flows through the heart. (c) Broken ground, and 100 µA flows through the heart in the opposite direction.
Examples of possible microshock incidents
Microchock via temporary
transvenous pacemaker
A figure from the second edition
Electrode Surface Area
Current density is the key
factor that causes VF.
Electrode area
VF probability ? ?
Threshold of VF
Figure 14.12 Thresholds of ventricular fibrillation and pump failure versus catheter area in dogs.
Conductive Surfaces
It only requires a small potential difference between two conductive surface
It doesn’t require a leakage current
To induce a microshock.
Electrode area
current density
VF more probable
Electrode area
electrode resistance
VF less probable
current magnitude
EEA018
Example 14.2
Macroshock
Macroshock:
Minimum current I for VF = 75 mA
Cross-sectional area A of the heart = 10 am 10 cm
Current density J = 75 mA/100 cm2 = 7.5 A/mm2
vs
Microshock
Microshock:
A = 90 mm2
I = 1000 μA
J = 1000 μA/90 mm2 = 11.1 μA/mm2
Conclusion: Macroshock & microshock cause VF
by the same mechanism
Figure 14.10 Thresholds of ventricular fibrillation and pump failure versus catheter area in dogs.
EE8016
Ground Potential Differences
Solution:
(1) A single patient grounding point
for all devices used in the vicinity of each patient
(2) Electrical isolation for all patient leads
Figure 14.11 (a) Large ground-fault current raises the potential of one ground connection to the patient. The microshock current can then flow
out through a catheter connected to a different ground. (b) Equivalent circuit. Only power-system grounds are shown.
14.6 Electrical-safety Codes and Standards
A code =法規, 行為準則,規範;
•a document that contains only mandatory requirements
• uses “shall”
• is cast in a form suitable for adoption into law by an authority that
has jurisdiction
• Explanations in a code must appear only in fine-print notes,
footnotes, and appendices.
A standard:
• contains only mandatory requirements
• Compliance tends to be voluntary.
• More detailed notes and explanations are given.
A manual or guide:
• doesn’t contain mandatory requirements
• Informative and tutorial
14.6 Electrical-safety Codes and Standards
An arduous history of the development, adoption, and use of
standards and codes for electrical safety in health-care
facilities:
1. Explosions and fires resulting from electric ignition of
flammable anesthetics
2. Microshock scare, 1970s, led to impractical proposals
3. Many years of debating over implicit requirements for
isolated-power systems and very low-leakage current
4. NFPA 99-1984 and ANSI/AAMI ES1-1985 standards were
adopted.
arduous 艱辛的
14.6 Electrical-safety Codes and Standards
NFPA = National Fire Protection Association
NASI = American National Standards Institute
AAMI = The Association for the Advancement of Medical Instrumentation
IEC = International Electrotechnical Commission)
The NFPA 99-1984
ANSI/AAMI ES1-1985
The NFPA 99Standard for Health Care Facilities2005
(Evolved from 12 NFPA documents that were combined in 1984 and revised
every 3 years)
•Electric equipment, gas, vacuum, environmental systems and materials
•The requirements for patient-care-related electric appliances
•The performance, maintenance, and testing of electrical equipment
•The performance, maintenance, and testing with regard to safety
•The safe use of high-frequency (100 kHz to microwave frequencies) electricity
14.6 Electrical-safety Codes and Standards
The National Electrical Code 2006, Article 517Health Care Facilities
A. General; B. Wiring design and protection; C. Essential electrical system; D.
Inhalation anesthetizing locations; E. X-ray installations; F. Communications,
signaling systems, data systems, fire-protective signaling systems, and systems
less than 120 Volts, nominal; G. Isolated power systems
ANSI/AAMI ES1 1993 Safe Current Limits for Electromedical
Apparatus
Chassis and patient lead leakage currents
NFPA = National Fire Protection Association
NASI = American National Standards Institute
AAMI = The Association for the Advancement of Medical Instrumentation
IEC = International Electrotechnical Commission)
IEC 60601-1 (2006) standard
Allows a “patient auxiliary current” up to 100 uA at not less than 0.1 Hz to permit amplifier bias
currents and impedance plethysmorgraphy if the current is not intended to produce a
physiological effect.
Table 14.1 Limits on Leakage Current for Electric Appliances
Electric Appliance
Chasis Leakage, uA
Patient-lead
Leakage, uA
not intended to contact patients
100
NA
not intended to contact patients and single
fault
500
NA
with nonisolated patient leads
100
10
with nonisolated patient leads and single
fault
300
100
with isolated patient lead
100
10
with isolated lead and single fault
300
50
plethysmorgraphy 體積變化描記
14.6 Electrical-safety Codes and Standards
Code vs standard
Code
Standard
yes
yes
Definition
Mandatory
Compliance
Explanation
14.7 Basic Approaches to Protection Against Shock
Protection against shock:
Method 1: Isolate and insulate patients from grounded
objects and electrical sources
Method 2: Maintain at the same potential all conductive
surfaces within the patient’s reach
Neither can be fully achieved in most practical
environments, so some combination of them must usually
suffice.
14.7 Basic Approaches to Protection Against Shock
Whom to protect?
1. Patients with accessible electrical connections to the heart.
(哀莫大於心死)
2. Patients with
reduced skin resistance
invasive connections
(e.g., coupled to electrodes)
(e.g., intravenous catheters)
exposure to wet conditions (e.g., dialysis, i.e., 洗腎)
3. Patients
4. Visitors and staff
Cost-benefit ratio:
safety vs purchase cost + maintenance cost
14.8 Protection: Power Distribution
Grounding system:
Essential requirement for protecting patients from both macroshock and microshock:
Low-resistance grounds that can carry current up to circuit-breaker ratings
(1) Macroshock:
(2) Microshock:
14.8 Protection: Power Distribution (cont.)
Grounding system: (cont.)
A good grounding system protects patients by :
(1) Keeping all conductive surfaces and receptacle grounds in the patient’s
environment at the same potential
(2) Protect the patients from ground faults at other locations (e.g., Fig. 14-11)
Grounding system, hierarchy of (see Fig. 14.14)
Patient-equipment grounding point
Reference grounding point
Building service ground
Figure 14.12 Grounding system All the receptacle grounds and conductive surfaces in the vicinity of the patient are connected to the patientequipment grounding point. Each patient-equipment grounding point is connected to the reference grounding point that makes a single
connection to the building ground.
Figure 14.12 Grounding system All the receptacle grounds and conductive surfaces in the vicinity of the patient are connected to the patientequipment grounding point. Each patient-equipment grounding point is connected to the reference grounding point that makes a single
connection to the building ground.
Figure 14.12 Grounding system All the receptacle grounds and conductive surfaces in the vicinity of the patient are connected to the patientequipment grounding point. Each patient-equipment grounding point is connected to the reference grounding point that makes a single
connection to the building ground.
14.8 Protection: Power Distribution (cont.)
Grounding system: (cont.)
Grounding system:
(1) connection 0.15
(2) diff. voltage (between receptacle ground & conductive surface) 40 mV
(3) The patient-equipment grounding point is connected individually to all
receptacle grounds, metal beds, metal door and window frames, water pipes,
and any conductive surfaces.
(4) Each patient-equipment grounding point
individually connected to a reference grounding point
connected to the building service ground
14.8 Protection: Power Distribution (cont.)
Isolated power-distribution system:
* High cost
* Only necessary in locations where flammable anesthetics are used
14.8 Protection: Power Distribution (cont.)
Ground fault circuit interrupters (GFCI):
Function:
= 0 ideally
If |Ihot conductor Ineutral conductor| 6 mA
Disconnect the electrical power source
(to prevent macroshock)
* Not sensitive enough to interrupt microshock level of leakage
current.
* Primarily for macroshock protection.
Note:
1.Microshock doesn’t need ground fault; leakage current can cause microshock.
2.Microshock level of leakage current < macroshock level of leakage current
14.8 Protection: Power Distribution (cont.)
Ground fault circuit interrupters (GFCI): (cont.)
•NEC (1996):
There shall be GFCIs in circuits serving
bathrooms, garages, outdoor receptacles, swimming pools, construction sites
•NFPA 99:
There shall be GFCIs in wet location, especially hydrotherapy areas, (where continuity of
power is not essential).
• In patient-care areas, circuits should not include GFCIs,
because: the loss of power to life-support equipment (due to GFCIs) may be more hazardous to
the patient than most small ground faults would be.
GFCI ($10)
This is attractive if brief
power interruptions can be
tolerated.
vs
isolated power-distribution system ($2000)
Figure 14.15 Ground-fault circuit interrupters (a) Schematic diagram of a solid-state GFCI (three wire, two pole, 6 mA). (b) Ground-fault
current versus trip time for a GFCI. [Part (a) is from C. F. Dalziel, "Electric Shock," Advances in Biomedical Engineering, edited by J. H. U.
Brown and J. F. Dickson IIII, 1973, 3, 223-248.)
http://www.elec-toolbox.com/Safety/safety.htm
N
G
H
Electric
device
GFCI
•When power is interrupted by a GFCI, the manual reset button on the GFCI must be pushed to restore
power.
• Most GFCIs have a momentary pushbutton that create a safe ground fault to test the interrupter.
Example 14.3
Most GFCIs have a momentary pushbutton that create a safe ground fault to test the interrupter. On Figure 14.15,
design the modification to permit this test.
Answer
14.9 Protection: Equipment Design
Reliable grounding for equipment
* Power cords: Hard Service (SO, ST, STO), Junior Hard Service (SJO, SJT, SJTO)
•Plugs: Avoid molded plugs (because of 40% to 85% invisible breaks within 1 to 10 years)
•Strain-relief devices
•Cord-storage compartment – to reduce cord damage
• Be careful of three-prong-to-two-prong adaptor
Reduction of leakage current (between chassis and patient leads)
*Low-leakage power cords
< 1.0 μA/m ---- are available
•Capacitor between the hot conductors and the chassis can be reduced thr layout and insulating
•Impedance from patient leads to hot conductors or chassis must be maximized
Double-insulated equipment
•Insulating material for the secondary insulation
•Safe even when spilled
insulation
14.9 Protection: Equipment Design
Operation at low voltage
(Use battery, < 10 V)
* e.g., inhalation-anesthetizing locations
Electrical isolation
. Different voltage sources and different grounds oneach side
. Isolation amplifiers: ohmic isolation > 10 M, isolation-mode voltage > 1000 V, CMRR > 100 dB
•Transformer/optical/capacitive isolation
CM
CMRR
Error
~
SIG
Isolation
barrier
ISO
Error
IMRR*
~
Isolation barrier
CR3
RF
i
~
CM
Isolation
Capacitance
and resistance
~
~
Input common
(a)
+
ISO
Output
common
o
=
SIG ±
CM
ISO
±
CMRR
IMRR
~ i
i3
i2
+V
AII
+
+
V
Input
control
Gain
*IMRR in v/v
AI
+
i1
RK = 1M
2
+o
RG
CR2
i2
1
ISO
+
+
i
CR1
(c)
o = i
RK
RG
o
Output
control
Isolation barrier
FB
AD202
In
In +
SIG
In com
+ISO
Out
-ISO
Out
(b)
+
Signal
±
Mod
Demod
Hi
±5V
F.S.
5V
F.S.
Lo
± 15 V (Driver)
o
Isolation
barrier
± 15 V (Receiver)
Power
+ 7.5 V
7.5 V
Rect and
filter
25 kHz
Oscillator
25 kHz
+ 15 V DC
Power
return
Analog
signal in, i
Freq
control
Osc
3 pF
Q
Q
3 pF
Frequency-to-
voltage converter
(phase-locked
loop)
Analog
signal out, o
(d)
Figure 14.14 Electrical isolation of patient leads to biopotential amplifiers (a) General model for an isolation amplifier. (b) Transformer
isolation amplifier (Courtesy of Analog Devices, Inc., AD202). (c) Simplified equivalent circuit for an optical isolator (Copyright (c) 1989 BurrBrown Corporation. Burr Brown ISO100) (d) Capacitively coupled isolation amplifier (Horowitz and Hill, Art of Electronics, Cambridge Univ.
Press. Burr Brown ISO106).
14.9 Protection: Equipment Design
Isolated heart connections
•Cardiac pacemakers powered by battery
•Blood-pressure sensors with triple insulation
•Catheters with conductive walls
Quiz: Which is safer? A catheter with insulated wall or
one with conductive wall? Why?
Ans:
14.10 Electrical-Safety Analyzer
Line Voltage
Cord Resistance
Case Leakage Current
Earth Leakage Current
Leads Leakage Current
Instrument Current
Insulation resistance
Earth resistance
Point-to-Point Measurement
14.11 Testing the Electric System
Electrical safety relies on the integrity of the power connection.
3-LED Receptacle Tester
Hot
Ground
Neutral
Open
The four possible states:
1. Hot (120 V)
2. GND
3. Open
4. Neutral
Possible practical cases: 43 = 64 cases
3-LED receptacle tester: 23 = 8 cases
120 V
☼
0V
◌
X
120 V
◌
☼
0V
☼
0V
◌
X
☼
0V
☼
120 V
☼
Figure 14.17 Three-LED receptacle tester Ordinary silicon diodes prevent damaging reverse-LED currents, and resistors limit current. The LEDs are ON for line voltages
from about 20 V rms to greater than 240 V rms, so these devices should not be used to measure line voltage.
Description (in textbook)
LEDs
1
2
Prongs
3
Hot
Ground
(Black) (Green)
Neutral
(White)
○ ○ ○ O
G
N
H
H
H
2. Neutral open
☼ ○ ○ H
G
O
3. No possible wiring
○ ☼ ○ ―
―
―
4. Ground open
○ ○ ☼ H
O
N
5. Hot/ground reversed
☼ ☼ ○ G
H
N
6. Correct (or ground/neutral reversed)
☼ ○ ☼ H
G
N
H
N
G
7. Hot/neutral reversed
○ ☼ ☼ N
G
H
8. Hot open and neutral/hot
☼ ☼ ☼ O
G
H
1. Hot open (or all hot)
Note:
The “correct wiring” is when Black = Hot, Green = Ground, and White = Neutral.
Tests of Grounding System in Patient-Care Areas
NFPA 99:
Between ground and receptacle:
< 0.1 ohm, new construction
< 0.2 ohm, existing construction
NFPA 99:
< 20 mV, new construction
< 40 mV, critical area
, existing construction
< 500 mV, general area
, existing construction
Tests of Isolated Power Systems
Alarm
Yes
No
3.7 mA
5.0 mA
Total hazardous current
(leakage current + LIM current)
14.12 Tests of Electric Appliances
Leakage current is the current that could flow from the point where a person makes contact with an appliance,
through that person's body, and back to ground (or some other point). [Jim Richards]
The leakage tests are commonly performed as the final production tests on medical appliances.
During a leakage test, the appliance is powered up under operating conditions.
The leakage test is not a common production test for most non-medical electrical appliances.
Various leakage tests are different in how or where the human body comes into contact with a medical
appliance.
The measuring device (such as a current meter in Figure 14.19) in a leakage test simulates the impedance of the
human body.
Tests include (1) normal power application (hot to 120 V and neutral to 0 V), (2) reverse power application (hot
and neutral reversed), (3) normal power with single fault, and (4) reverse power with single fault .
Tests on single faults are essential because it is a problem that could occur. Two or more faults are unlike to
happen, so tests on them are not considered necessary.
Source: Jim Richards, Medical Electronics Ensuring Compliance with Product Safety Tests, 2002 Reference Guide (Compliance
Engineering Magazine ) , http://www.ce-mag.com/archive/02/Spring/richards.html
Ground-Pin-to-Chassis Resistance
Figure 14.18 Ground-pin-to-chassis resistance test
Chassis Leakage Current
Appliance power switch
(use both OFF and ON positions)
Open switch
for appliances
not intended to
contact a patient
Grounding-contact
switch (use in
OPEN position)
Polarity- reversing
switch (use both
positions)
Appliance
H (black)
To exposed conductive
surface or if none, then 10 by
20 cm metal foil in contact
with the exposed surface
H
N
120 V
N (white)
G (green)
Building
ground
G
Insulating surface
I
Current meter
This connection is at
service entrance or on
supply side of
separately derived
system.
Test circuit
H = hot
N = neutral (grounded)
G = grounding conductor
simulates the human body
I < 500 μA for facility owned housekeeping and maintenance appliances
I < 300 μA for appliances intended for use in the patient vicinity
(a)
900
Input of
test load
1400
0.10 F
100
15
mV
Millivoltmeter
Leakage current
being measured
(b)
Figure 14.19 (a) Chassis leakage-current test. (b) Current –meter circuit to be used for measuring leakage current. It has an input impedance of 1
k and a frequency characteristic that is flat to 1 kHz, drops at the rate of 20 dB/decade to 100 kHz, and then remains flat to 1 MHz or higher.
(Reprinted with permission from NFPA 99-1996, "Health Care Facilities," Copyright © 1996, National Fire Protection Association, Quincy, MA
02269. This reprinted material is not the complete and official position of the National Fire Protection Association, on the referenced subject,
which is represented only by the standard in its entirety.)
Ammeter Design
An ammeter is placed in series with a circuit element to measure the electric current flow through it. The meter
must be designed offer very little resistance to the current so that it does not appreciably change the circuit it is
measuring. To accomplish this, a small resistor is placed in parallel with the galvanometer to shunt most of the
current around the galvanometer. Its value is chosen so that when the design current flows through the meter it
will deflect to its full-scale reading. A galvanometer full-scale current is very small: on the order of milliamperes.
galvanometer 檢流計(測驗微小電流、電壓、電量),
Source: http://hyperphysics.phy-astr.gsu.edu/hbase/magnetic/ammet.html
The input impedance of the current meter in Figure 14.18
% Matlab code for ploting the input impedance of current meter
R1 = 900; R2 = 100; R3 = 1400; R4 = 15; C1 = 0.10e-6;
f = [1e0, 1e1, 1e2, 1e3, 1e4, 1e5, 1e6, 1e7, 1e8]
Z_volmeter = 1./(j*2*pi.*f*C1) + R4
Z_total = R1 + 1./(1/R2 +1./(R3 + Z_volmeter))
Z_total_mag = abs(Z_total)
Z_volmeter_mag = abs(Z_volmeter);
subplot(2,1,1);
semilogx(f,Z_total_mag);
title('Input impedance of current meter');
xlabel = ('Frequency, Hz'); ylabel = ('Magnitude, ohm');
subplot(2,1,2);
semilogx(f,Z_volmeter_mag);
title('Impedance across volmeter');
xlabel = ('Frequency, Hz'); ylabel = ('Magnitude, ohm');
Input impedance of current meter
1000
999
998
997
996
995
994
993
0
10
1
10
2
10
6
2
3
10
4
10
5
10
6
10
7
10
8
10
Impedance across volmeter
x 10
1.5
1
0.5
0
0
10
1
10
2
10
3
10
4
10
5
10
6
10
7
10
8
10
Lakage current in Patient Leads
Figure 14.19 Test for leakage current from patient leads to ground (Reprinted with permission from NFPA 99-1996, "Health Care Facilities,"
Copyright © 1996, National Fire Protection Association, Quincy, MA 02269. This reprinted material is not the complete and official position of
the National Fire Protection Association , on the referenced subject, which is represented only by the standard in its entirety.)
Test for leakage current between patient leads
Figure 14.21 Test for leakage current between patient leads (Reprinted with
permission from NFPA 99-1996, "Health Care Facilities," Copyright © 1996, National Fire Protection Association, Quincy, MA
02269. This reprinted material is not the complete and official position of the National Fire Protection Association , on the
referenced subject, which is represented only by the standard in its entirety.)akage current between patient leads
Test for ac isolation current
Figure 14.22 Test for ac isolation current (Reprinted with permission from NFPA 99-1996, "Health Care Facilities,"
Copyright © 1996, National Fire Protection Association, Quincy, MA 02269. This reprinted material is not the
complete and official position of the National Fire Protection Association , on the referenced subject, which is
represented only by the standard in its entirety.)
CONCLUSION
To achieve adequate electrical safety in health-care
facilities:
. A good power distribution system
. Careful selection of well designed equipment
. Periodical testing of power systems and equipment
. Modest training program for medical personnel
• Scope: Ch 6, partial ch 7, partial ch 8
Ch 13, ch 14