Chapter 19
advertisement
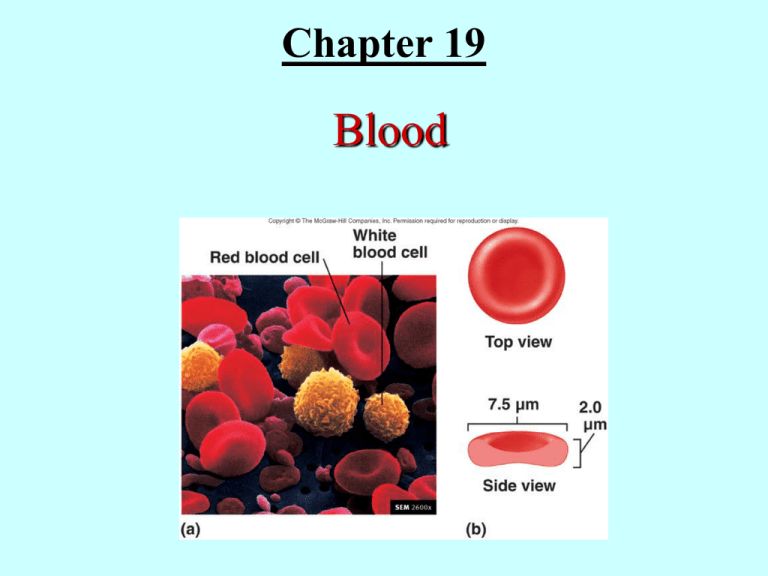
Chapter 19 Blood Functions of Blood • Transport of: – Gases, nutrients, waste products – Processed molecules – Regulatory molecules • • • • Regulation of pH and osmosis Maintenance of body temperature Protection against foreign substances Clot formation Blood is circulated by pumping action of the heart, the valves in blood vessels and the contracting action of calf muscles. The total blood volume of an adult female is 4 - 5 L, while that of an adult male is 5 - 6 L. If a person loses more than 1/3 of his blood, his life will be in danger. Blood constitutes about 8% of the total body weight of the human and the components may be divided with centrifugation. Composition of Blood 3. Blood collection and analysis Collection of human blood is usually performed from a superficial vein via a venipuncture or from the fingertip or the sole. Only when needed an arterial puncture may be performed. The temperature of blood is about 38˚C and is slightly higher than that of the body temperature. Having a large quantity of proteins in plasma (7g/100 ml) and corpuscles, blood viscosity is more than five times higher than that of water. The pH of blood is about 7.4. a. Differences between plasma and interstitial fluid The composition of the plasma and that of interstitial fluid is about the same, but the former has more proteins and dissolved gases. b. Plasma proteins 7 g/100ml of plasma are plasma proteins. Albumin: 58% of plasma proteins. Osmotic balance. Globulin: 38%. Immunoglobulins, lipoproteins and transport proteins. Antibodies and thyroid-binding proteins. Fibrinogen: 4%. Can form large fibrins to form blood clot. The 50% of plasma proteins are made in the liver. Immunoglobulins are produced by plasma cells. c. The other substances in plasma In addition of dissolved proteins, plasma contains ions, nutrients, waste products, gases and regulatory substances. Formed Elements • Red blood cells (erythrocytes) • White blood cells (leukocytes) – Granulocytes • Neutrophils • Eosinophils • Basophils – Agranulocytes • Lymphocytes • Monocytes • Platelets (thrombocytes) The hematocrit is about 46% for the males and about 42% for the females. Red blood cells - 95% of the formed elements in volume or 4.2 - 6.2 millions/mm3. Erythrocytes are enucleated and have little organelles White blood cells (leukocytes) - Have nuclei Granulocytes are: neutrophils, lymphocytes, monocytes, eosinophils and basophils Platelets - Enucleated and have little organelles Production of Formed Elements • Hematopoiesis or hemopoiesis: Process of blood cell production • Stem cells: All formed elements derived from single population – Proerythroblasts: Develop into red blood cells – Myeloblasts: Develop into basophils, neutrophils, eosinophils – Lymphoblasts: Develop into lymphocytes – Monoblasts: Develop into monocytes – Megakaryoblasts: Develop into platelets Hematopoiesis The major production sites of the formed elements shift: The first 8 weeks: They start at the embryonic yolk sac and they begin to settle in the liver, spleen, thymus, and bone marrow. They become stem cells. From the 8th week to fifth month: In the liver and spleen are the primary sites of Hemopoiesis. After the birth and among children: In most of the red bone marrow. In the adult: In the red bone marrow of skull, ribs, sternum, vertebrae, pelvis, proximal femur and proximal humerus. Observe the hematopoiesis of stem cells in Fig. 19.2. Stem cells are the origin of all formed elements. Note the types of blast cells and the final cell types produced. Erythrocytes • Structure – Biconcave, anucleate • Components – Hemoglobin – Lipids, ATP, carbonic anhydrase • Function – Transport oxygen from lungs to tissues and carbon dioxide from tissues to lungs Red blood cells contain: Hemoglobin, which binds oxygen at its heme (Oxyhemoglobin) and carbon dioxide at the N-terminal amino group as (carbaminohemoglobin), No nucleus or organelles, Thus, only glycolytic enzymes to form energy by Glycolysis. Carbonic anhydrase to transport carbon dioxide. CO2 + H2O ---- H2CO3 == H+ + H2CO3Phospholipids and membrane proteins. Others: ATP, enzymes, 2,3-diphosphoglycerate RBC are: 95% in volume of the formed elements. 5.4 million cells/one microliter (mm3) of blood for a man 4.8 for a woman. 260 million RBC/drop of blood 25 trillion RBC in the blood of an adult = 1/3 of all the cells in the human. The difference in the hematocrit mention earlier, i.e. 46 to men and 42 to women, arises from the fact that androgens in men stimulate erythropoiesis, while estrogens in women are inhibitory. The ratio of white cells to red cells is 1 to 1000. The hematocrit vs. disease: Anemia and polycythemia The structure of RBC Uniquely biconcave and flexible RBC (Fig. 19-2), have excellent exchange of gases between the cells and the environment. Contrary to a sphere, the RBC has the maximum surface to volume ratio. The diameter is 7.5 microns and the thickness varies at the edge (thick, 1.5 microns) and the center (thinner, 1 micron) making it possible to tumble and bend in tissue capillaries. ii. The primary function of RBC is carried by Hemoglobin 33% of RBC is hemoglobin, Hb, an oxygen and CO2 carrying protein. Each Hb consists of two pairs of subunits (alpha and beta) and each subunit has an oxygen binding heme. (Fig. 19-3) Since the oxygen binding to heme is reversible, the number of oxygen bound to heme depends upon the amount of oxygen in the environment of Hb. Thus, in the lungs, where oxygen pressure is high, Hb binds oxygen and carry the gas to the tissues where the oxygen pressure is low. Binding of CO2 to Hb is not at the heme, but is at the alpha amino group of the N-terminal ends of four subunits Binding of CO2 to Hb is not at the heme, but is at the alpha amino group of the N-terminal ends of four subunits. CO2 binding is essentially opposite to that of oxygen, but again follows the amounts of CO2 in plasma. The circulation of CO2 also relies on the chemically dissolved form of CO2, i.e., bicarbonate. This process is facilitated by carbonic anhydrase. Thus, carbon dioxide may be transported by: as carboamino hemoglobin, dissolved bicarbonate and free carbon dioxide. iii. Life span and circulation Complete circulation of an erythrocyte in a body usually takes less than a minutes. During this period, especially while negotiating through tissue capillaries of less than several microns of diameter, pulsating motion of blood flow severely stresses the erythrocytes. In addition, despite the presence of complex protective mechanisms, carrying oxygen provide ample opportunities to cause oxidative damages to the contents of the cell. As a consequence, the life span of a red blood cell is about 120 days. Since the hematocrit of a normal person is relatively consistent, the loss of erythrocytes is compensated with continuous erythropoiesis. (Fig. 19-5,6) Old erythrocytes are usually phagocytically broken down in the liver, spleen, bone marrow. Released Hb, when it is a small quantity, will path through the kidneys to the urine. If this level goes up, there will be coloration of the urine - hemoglobinuria. Erythropoiesis • Production of red blood cells – Stem cells proerythroblasts early erythroblasts intermediate late reticulocytes • Erythropoietin: Hormone to stimulate RBC production Recycling of RBC/hemoglobin components is as follows: (Seeley Fig. 19.6) Macrophage in the spleen, liver and other lymphatic tissues phagocytically engulf erythrocytes. Globular proteins are broken down to amino acids for resumption. Heme is separated form its iron and becomes biliverdin (green) then to bilirubin to be absorbed in the livers. Excrete it in the bile. jaundice. Iron may be stored with the plasma protein, transferrin and recycled. Hemoglobin Breakdown iv. Erythropoiesis When oxygen pressure in blood is lowered, erythropoiesis in human adults starts in the red marrow of vertebrae, sternum, ribs, skull, scapulae, pelvis and proximal limb bones. (Fig. 19-5) Note the sequence of events in Fig. 19-6 and pay attention when enucleation occurs. Hemocytoblasts - myeloid stem cells - proerytrhoblast erythroblast stages - reticulocyte - erythrocyte Erythropoiesis is regulated with erythropoietin from the kidneys, which appears in the plasma when peripheral tissues are exposed to low oxygen concentration, hypoxia. c. White blood cells - Leukocytes They are different from RBC because of their nuclei and lack of hemoglobin. They are loosely divided into: (Table 19-3/Fig. 19-11) Granulocytes: neutrophils, eosinophils, basophils Agranulocytes Monocytes, lymphocytes As many as 6 - 8,000 leukocytes in 1 microliter of blood, but most of the leukocytes are found in peripheral tissues. ii. General functions . General defense: neutrophils, eosinophils, basophils and monocytes Specific immunity: Lymphocytes iii. Neutrophils: Polymorphonuclear Live in the circulation for only 10 - 12 hours, then move into tissues, where they live up to 1 - 2 days. Phagocytic and secrete lysozymes to digest bacteria and others iv. Eosinophils v. Basophils Reduce inflammation Releases histamine, which promotes inflammation Releases heparin, which inhibits b lood clotting. vi. Monocytes Live 2 - 3 days in circulation and to tissues as macrophages Phagocytes foreign bodies. Increased number of monocytes is an indication of infection. vii. Lymphocytes survive years About the same size as RBC and has a large nucleus. Most of lymphocytes dwell in the lymphatic system. There are three types: 1. T cells: Attack foreign bodies 2. B cells: Differentiate into plasma cells, which secrete antibodies 3. Natural Killer cells (NK cells): Destroy body’s own abnormal cells Thrombocytes • Cell fragments pinched off from megakaryocytes in red bone marrow • Important in preventing blood loss – Platelet plugs – Promoting formation and contraction of clots c. Platelets Megakaryocytes in bone marrow release their fragments into circulation, which are called platelets. Platelets have no nuclei. Participate in blood clotting. Platelets survive about 10 - 12 days in circulation and are about 150,000 - 300,000 /uL. Thrombocytopenia is a loss of platelets and is a sign of bleeding etc. Thrombocytosis is excess platelets and is a sign of infection etc. Hemostasis • Arrest of bleeding • Events preventing excessive blood loss – Vascular spasm: Vasoconstriction of damaged blood vessels – Platelet plug formation – Coagulation or blood clotting 6. Hemostasis - arrest of bleeding Prevents loss of blood in three phases: The vascular phase: Immediate temporary closure of a blood vessel by contraction of vascular smooth muscles. The platelet phase: Formation of a platelet plug by platelet adhesion and aggregation (Fig. 19-13 and 14) The coagulation phase: For a large blood clot formation by the network of fibrin from fibrinogen. A large number of steps involving many factors are required, some of which require thrombin and Ca++. Platelet Plug Formation Coagulation • Stages – Activation of prothrombinase – Conversion of prothrombin to thrombin – Conversion of fibrinogen to fibrin • Pathways – Extrinsic – Intrinsic a. The clotting process Clotting is the phenomenon where blood cells are trapped in the framework of fibers. (Seeley Fig. 19.10, 11) The clotting process requires calcium and 11 different plasma proteins, mostly enzymes. The final important step is formation of fibrin from fibrinogen. Once the process is triggered by tissue factor of damaged endothelial cells, by exposing collagen fibers or rough surface, the enzymes are successively activated to complete the clotting process - a cascade. The extrinsic pathway is fast, 15 seconds, but the slower intrinsic pathway add further extensive aggregation. Thromboplastin formed by either of these pathways triggers the common pathway that completes the coagulation process by converting fibrinogen to fibrin. Clot Formation b. Clot retraction and removal The platelets begin to contract - clot retraction. (Seeley Fig. 19.12) During repair process of tissue, the clot gradually dissolve fibrinolysis. The process draws much attention, since dissolving clots in the heart attack or stroke is clinically important. To dissolve clot: Activate plasminogen by tissue plasminogen activator (t-PA). --Plasmin is produced. --- Plasmin digests the fibrin strands to dissolve the clot. Fibrinolysis • Clot dissolved by activity of plasmin, an enzyme which hydrolyzes fibrin Blood Grouping • Determined by antigens (agglutinogens) on surface of RBCs • Antibodies (agglutinins) can bind to RBC antigens, resulting in agglutination (clumping) or hemolysis (rupture) of RBCs • Groups – ABO and Rh 7. Blood types Genetically determine RBC antigens rest on the surface of the membrane. There are at least 50 different kinds of antigens on the surface of an RBC. Their antibodies are found in plasma. One set of important antigens are A and B, though type A/B antibodies are not found in the blood until about 2 months after birth. (Fig. 19-8) ABO type. Agglutination Reaction Blood donor and recipient (Seeley Fig. 19.14) Type O subject, who has no surface A/B antigen, has been considered as a universal donor, since the donated RBC will not be coagulated. However, the antibodies in the plasma can interact with the surface antigens of the recipient and may induce minor reactions. Thus, the word “universal donor” is misleading. Rh Blood Group • First studied in rhesus monkeys • Types – Rh positive: Have these antigens present on surface of RBCs – Rh negative: Do not have these antigens present • Hemolytic disease of the newborn (HDN) – Mother produces anti-Rh antibodies that cross placenta and cause agglutination and hemolysis of fetal RBCs Diagnostic Blood Tests • Type and crossmatch • Complete blood count – Red blood count – Hemoglobin measurement – Hematocrit measurement • White blood count • Differential white blood count • Clotting Blood Disorders • Erythrocytosis: RBC overabundance • Anemia: Deficiency of hemoglobin – – – – – Iron-deficiency Pernicious Hemorrhagic Hemolytic Sickle-cell • • • • • • Hemophilia Thrombocytopenia Leukemia Septicemia Malaria Infectious mononucleosis • Hepatitis 8. Sickle cell anemia (Fig. 19-4) Genetic disease originated from a point mutation leading to a replacement of 7th amino acid in the beta chain, glutamic acid, to valine. Upon removing oxygen, sickle cell hemoglobin polymerizes to form hard bundles, thus leading to a deformation of cells. The cells may clog the blood capillaries to trigger occlusion, thus the onset of sickle cell episode – a severe pain. Cells live only 20 -30 days, Hct close to 25% May be treated with blood transfusion, injection of hydroxyurea, or bone marrow transplant. Sickle cell episode is observed only among the homozygous patients and heterozygous patients show little sign of the disease.