Haemolytic Uraemic Syndrome
advertisement
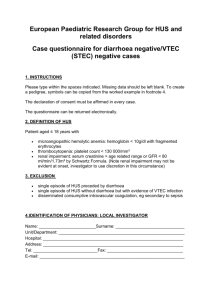
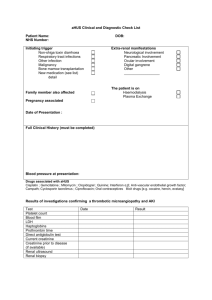
Haemolytic Uraemic Syndrome David V Milford Paediatric Nephrology for the General Paediatrician 2012 Manchester Overview • • • • • Presentation Diagnosis Management Prognosis and follow-up Atypical HUS Haemolytic uraemic syndromes in childhood Syndrome comprising acute renal failure of varying severity microangiopathic anaemia thrombocytopenia of varying severity Multiple aetiologies BPSU National HUS study 1985-1988 D+ 282 (94.6%) 165 (59%) D16 (5.4%) 9 (56%) followed for > 4 months 259 15 lone hypertension CRF ESRF died 3 17 0 13.6% 15 2 2 5 3 reported dialysed Arch. Dis. Child 1990; 65:716-721 78% Arch. Dis. Child 1990; 65:716-721 Evolution of lab results in HUS – outbreak in an institution Diagnosis • Diarrhoea (often bloody) • Haematological – microangiopathic haemolytic anaemia - thrombocytopenia Fragmented red cells Absence of platelets Acute Kidney Injury Shiga toxin producing E.coli (STEC) isolates BAPN/CDC study 1985-88 isolates VTEC O157 HUS 185 60 39 Bloody diarrhoea 48 4 3 Diarrhoea 54 3 1 Controls 46 2 0 Arch. Dis. Child. 1990; 65:722-727 D+ HUS and EHEC • EHEC colonise cattle • Transmission – contaminated meat, milk, water, fruit, vegetables • Exposure to EHEC → diarrhoea in ≈ 10% children • HUS develops in ≈ 15% of children with EHEC diarrhoea • O157:H7 predominant serotype in the UK – O26:H11, O103:H2, O111:NM, O121:H19, O145:NM Annual STEC cases in the UK Emerging Infectious Diseases 2005; 11: 590-6 Non-renal complications • Seizures – hyponatraemia – neurotoxicity (STx receptors – neurones, endothelium) • Hypertension • Gut – rectal prolapse – toxic megacolon, perforation, intussception • Cardiomyopathy • Diabetes mellitus Acute CNS changes 6 months Even in patients with severe CNS involvement on acute imaging studies, prognosis can be favourable for clinical outcome and resolution of pathological imaging findings Pediatr Radiol (2004) 34: 805–810 Clin J Am Soc Nephrol 2010; 5:1218–1228, Rectal prolapse Air in bowel Late change - stricture Emerging Infectious Diseases 2005; 11: 590-6 Infections in HUS 1997-2001 395 D+ HUS 1 O26 65 18 D- HUS 329 (83%) O157 +ve culture/serology No infection identified 59 S pneumonae 7 Campylobacter 2 Shigella Sonnei 1 S pneumonae 1 Staph aureus 1 Emerging Infectious Diseases 2005; 11: 590-6 CKD 1 Died 2 (out of 8 cases) Northern German outbreak May-July 2011 • • • • Source: bean sprout farm in Lower Saxony Sprouted from batch of seeds from Egypt 3793 cases of diarrhoea – O104:H4 Delay in symptoms, ingestion → diarrhoea 8 days • 827 (22%) developed HUS, 88% in adults • 53 deaths • 2010 European data – 4000 STEC cases reported, 5.5% developed HUS – O157 (41%), 026 (7%), O103 (2.5%) Management • Conservative – Monitor fluid balance, sodium, potassium, H+,BP – Furosemide may be useful early – Sodium, protein restriction; high calorie intake – Transfuse with caution – Avoid antibiotics/anti-motility agents/NSAID • Transfer to regional centre – Oliguria + • Fluid overload, need for transfusion, high K – Anuria – Complications of D+ HUS Prognosis and follow-up • BCH (n=250) 56% required acute dialysis • Prognostic markers – Neutrophils >20 at presentation – Dialysis > 2weeks • Mortality – 5% (BPSU 1985-88) – 1.8% (BPSU 1997-2001) • Long term: HBP, reduced GFR, proteinuria – Variable in studies, probably 20-30% – BCH n=201 19% poor outcome at 5,10,0r 15 yrs Proteinuria at 1 year and outcome Poor outcome Good outcome J Pediatr 1991; 118:191-4 • Follow-up – Frequently until Hb and creatinine normal – BP, PCr and EMU protein at 1 year after illness – BP, EMU protein, formal GFR, renal USS at 5 years and every 5 years until post pubertal – BP, EMU protein by GP at intervals once discharged • Lifestyle advice – Avoid overweight, high sodium intake – Avoid smoking – Girls need renal function/proteinuria monitoring during pregnancy Level 1: aetiology advanced 1.i Infection induced (a) Shiga and shiga-like toxin-producing bacteria; enterohaemorrhagic Escherichia coli, Shigella dysenteriae type 1, Citrobacter freundii (b) Streptococcus pneumoniae, neuraminidase and T-antigen exposure 1.ii Disorders of complement regulation (a) Genetic disorders of complement regulation (b) Acquired disorders of complement regulation, e.g. anti-factor H antibody 1.iii von Willebrand proteinase, ADAMTS13, deficiency (a) Genetic disorders of ADAMTS13 (b) Acquired ADAMTS13 deficiency; autoimmune, drug induced 1.iv Defective cobalamin metabolism 1.v Quinine induced Level 2: aetiology unknown 2.i Human immunodeficiency virus (HIV) 2.ii Malignancy, cancer chemotherapy and ionising radiation 2.iii Calcineurin inhibitors and transplantation 2.iv Pregnancy, HELLP syndrome and oral contraceptive pill 2.v Systemic lupus erythematosus and antiphospholipid antibody syndrome 2 vi Glomerulopathy 2.vii Familial, not included in part 1 2.viii Unclassified Typical/diarrhoeal/ D+ HUS Atypical/ non-diarrhoeal/ D- HUS Alternative complement pathway Johnson, Eur J Pediatr 2008:167;965–971 Non-diarrhoeal HUS • Requires urgent referral to a nephrology centre • Associated with – High risk of death, CKD, hypertension, CNS events, recurrent episodes, familial • Therapies used – Plasmapheresis – Plasma infusion (especially ADAMTS13) – Eculizumab (binds to C5 and blocks C5 convertase) – Liver, liver/kidney transplantation QUESTIONS? Glomerular size in HUS patients with proteinuria 3.3-7 years after illness n=7 J Pediatr 1998; 133:220-3