Powerpoint Overheads
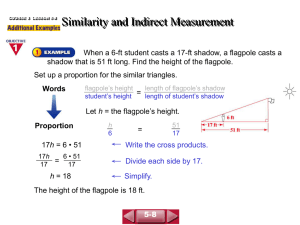
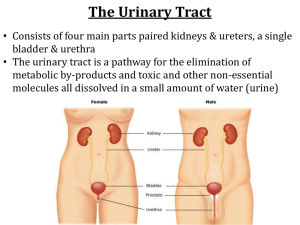
advertisement

Microscopic Urinalysis Vicki S. Freeman, Ph.D Clinical Laboratory Methods General Considerations • The results of the microscopic should correlate with physical and chemical test results. • Contamination is common; especially in voided specimens when no effort is made to obtain a “clean catch” specimen. • Results more reliable with concentrated, but fresh specimen, as cellular elements tend to lyse in dilute, hypotonic urine or alkaline urine. More General Considerations • Urine should be examined within one hour of collection. If not, specimen should be refrigerated. • Normal values vary considerably due to variation in concentration of the specimen and different methods used to concentrate the sediment by centrifugation (volume, speed, etc.) Sediment Preparation & Procedure 1 Centrifuge 10 ml of well-mixed urine specimen (1500-2000 rpm) for 5 minutes. 2 Suction or pour off all but 1.0 ml of urine 3 Resuspend sediment and place approximately .05 ml on a glass slide - add coverslip on top Sediment Preparation & Procedure • Examine under low power with dimmed light or with phase contrast microscopy to estimate urine sediment (casts and crystals). Report numbers per low power field (LPF). • Examine under high power objective to estimate #s of RBCs, WBCs, and renal tubular epithelial cells (RTE); report per high power field (HPF). Typical Urine Report on Normal Male • • • • • • • • • • • Specific Gravity pH range Protein Glucose Ketones Urobilinogen Bilirubin Occult Blood WBC Esterase Nitrite 1.020 4.8 - 7.5 Negative Negative Negative 0.8 EUs Negative Negative Negative Negative • Color • Appearance Straw Clear • Microscopic • • • • • • 0-8 WBC/HPF 0-2 RBC/HPF 0-1 Hyaline Cast Few Bacteria 0-1 RTE/HPF Few Ca oxalate crystals Epithelial Cells • • • • • Squamous epithelial cells Transitional epithelial cells Renal tubular epithelial cells Oval Fat Bodies Clue Cells Squamous Epithelial Cells • • • • 30-50 microns large, flat cells with small nuclei Appear flat with abundant cytoplasm Originate from the superficial lining of the urethra and vagina • Common contaminant; seen in female voided specimen Transitional epithelial cells • 20 -30 microns • Polyhedral shaped but swell in urine to spheroidal shape • Have round or pear-shaped contours with small central nucleus (may be bi-nucleated) • Originate from transitional epithelial lining of the renal pelvis, ureter, urinary bladder and proximal urethra • A few are seen in normal urine; large clumps suggest possible carcinoma. Renal tubular epithelial cells (RTE) • 14 - 60 microns from proximal and distal convoluted tubules • Single, oblong or egg-shaped cells with coarsely granular eosinophilic cytoplasm • Nuclei may be multiple but are small with dense chromatin • Seen in cases of acute tubular necrosis and drug or heavy metal toxicity Oval Fat Bodies • Renal tubular cells that have absorbed lipids. • Are highly refractile and produce a characteristic Maltese cross appearance with polarized light. • Extremely significant finding. Seen in lipid nephrosis and terminal kidney disease. Clue Cells • Squamous epithelial cells covered with coccobacilli, Gardnerella vaginalis Blood Cells • Red Blood Cells • White Blood Cells Red Blood Cells • Normal size 6-8 microns, biconcave discs • Swollen in hypotonic, crenated in hypertonic urine • Empty RBC membranes may be seen from lyzed cells in alkaline urine • Confusing artifacts • oil droplets, yeast, urates Red Blood Cells • Normal – Male – Female 1-2 RBC/HPF 3-12 RBC/HPF • Increased RBC seen in – Renal disease such as glomerulonephritis, lupus nephritis, kidney stones, tumors and trauma – Lower urinary tract disease such acute and chronic infection, tumors and strictures – Extrarenal disease such as acute appendicitis. White Blood Cells • 10-12 microns, swell to 15 microns in alkaline or hypotonic urine, nuclei more distinct in acid urine • Mainly neutrophils and have a granular cytoplasm and lobed nucleus White Blood Cells • Normal 0-8 WBC/HPF • Increased in – pyelonephritis, cystitis, urethritis, prostatitis • “Glitter cell” term used to describe large WBC seen in hypotonic urine that have Browian movement of granules in cytoplasm • Clumps of WBCs considered very significant in indicating an infection Other Urinary Elements • Bacteria • Yeast – confused with red cells – look for budding, doubly refractive wall • Trichomonas – confused with white cells – look for undulating membrane movement • Sperm Urine Casts • • • • • • • • Hyaline Casts Red Blood Cell Casts Hemoglobin or Blood Cell Casts White Blood Cell Casts Renal tubular epithelial cell casts Granular casts Waxy casts Fatty casts Urinary Casts • Cylindrical structure which consists of – jelled protein (Tamm-Horsfall mucoprotein) – clumping of the protein or conglutination of material within the lumen of the renal tubules – Albumin or globulins may be mixed with the mucoprotein • Conditions that increase urine cast formation – – – – Increased concentration of the urine] Increased acidity of the urine High protein concentration in the urine Stasis or obstruction of the nephrons by cells or debris Hyaline Casts • Formed in the lumen of the distal convoluted tubules or collecting ducts and serve as the matrix of all casts • Pale, smooth and usually cylindrical, homogeneous gel-like forms of low refractive index. Mainly Tamm-Horsfall mucoprotein • Narrower casts form in the convoluted tubules while broader casts form in the collecting ducts. Red Blood Cell Casts • • • • These casts are always pathologic Diagnostic of glomerular disease or damage Classically found in acute glomerulonephritis RBC outline must be sharply defined in at least part of the cast Hemoglobin Cast • An RBC cast in which the red cells have ruptured and disintegrate • Cast appears reddish-brown due to acid hematin formation • Diagnostic of glomerular disease or damage such as acute glomerulonephritis WBC Cast • Hyaline cast with WBCs embedded in matrix • Indicate inflammation/infection in kidney • Seen in acute pyelonephritis and other nephritis conditions Renal Tubular Epithelial Cast • Hyaline cast with renal tubular epithelial cells embedded in the hyaline matrix • Form as result of stasis and necrosis of the tubules • Seen in severe chronic renal disease, exposure to nephrotoxic agents or viruses and rejection in kidney transplants Granular Casts • Results of the degeneration of cellular components of casts or direct aggregation of serum proteins into a matrix of TammHorsfall mucoprotein • Usually indicates significant renal disease • Thought to be the result of breakdown of cellular casts with the progression of cellular to coarsely to finely granular to waxy. Waxy Casts • Smooth, homogeneous, highly refractive appearance. Typically have blunt, broken ends and cracked or serrated edges • Seen in patients with severe chronic renal failure, malignant hypertension, diabetic nephropathy • May also be seen in acute renal disease and renal allograft rejection Fatty Casts • Casts that have incorporated either free fat droplets or oval fat bodies. • In the fat is cholesterol, the droplets will be demonstrate a “Maltese cross” appearance under polarized light. • Droplets which consist of triglycerides or neutral fat will not polarize but will stain with Sudan III or Oil Red O stains for fat. Crystals seen in Acidic Urine • Calcium oxalate – envelope, dumbbell or ring forms – colorless, do not polarize – Common cause of kidney stones • Uric acid – rhombic plates, rosettes, wedges, needles – polarize to multicolored – found in gout • Amorphous urates – clumps of brownish-yellow granules Crystals seen in Alkaline Urine • Triple phosphate – Coffin lid crystals – colorless prisms • Ammonium biurate – thorn-apple crystals – yellow-brown, spicule covered spheres Crystals with Pathogenic Significance • Cystine – colorless hexagonal plates – do not polarize – associated with inborn errors of metabolism • Cholesterol – rectangular plate with a notched corner or edge – polarize as multicolored plates – seen in nephritis and nephrosis conditions Gladys Glomerulus (35 yr old) • • • • • • • • • • • • Color Appearance Specific Gravity Glucose Bilirubin Ketone Blood pH Protein Urobilinogen Nitrite Leukocytes Pale Clear 1.035 Neg Neg Neg Neg 5.0 1+ 0.2 Neg Trace • • • • • Epi cells Many Casts 2-5 Hyaline RBCs/HPF 0-2 WBCs/HPF 10-25 Crystals 2-5 Triple PO4 Many Amorp Urates • Bacteria Few (10-50) Tammy Tubule (25 yr old) • • • • • • • • • • • • Color Appearance Specific Gravity Glucose Bilirubin Ketone Blood pH Protein Urobilinogen Nitrite Leukocytes Yellow Cloudy 1.003 Neg Neg Neg Neg 8.5 4+ 0.2 Neg Trace • • • • • Epi cells 5-20 Casts None RBCs/HPF 50-100 WBCs/HPF 0-2 Crystals Many Amorp Urates • Bacteria None Bowman S. Capsule (2 yr old) • • • • • • • • • • • • Color Appearance Specific Gravity Glucose Bilirubin Ketone Blood pH Protein Urobilinogen Nitrite Leukocytes Yellow Hazy 1.011 Neg Neg Neg Neg 5.0 Neg 0.2 Pos Mod • Epi cells Few • Casts 2-5 Hyaline 5-10 Fine gran >10 Coarse gran • RBCs/HPF 2-5 • WBCs/HPF None • Crystals Few Amorp Urates • Bacteria None Ned Nephron (23 yr old) • • • • • • • • • • • • Color Appearance Specific Gravity Glucose Bilirubin Ketone Blood pH Protein Urobilinogen Nitrite Leukocytes Amber Clear 1.006 Neg Neg Small Mod 6.0 Neg 1.0 Positive Mod • • • • • • • Epi cells >100 Casts None RBCs/HPF None WBCs/HPF 25-50 Crystals None Bacteria Mod (50-200) Other Budding yeast Renal Diseases • • • • Nephrosis Cystitis Acute pyelonephritits Acute glomerulonephritis Sediment Procedure Centrifuge 10 ml of well-mixed urine specimen (1500 2000 rpm) for 5 minutes Pour off all but 1.0 ml of the urine Resuspend sediment and place approximately 0.05 ml on a glass slide and add coverslip Examine under low power with dimmed light to estimate urine sediment (casts and crystals). Report numbers per low power field (lpf) Examine under high power to estimate #s of RBCs, WBCs and renal tubular epithelial cells; report per high power field (hpf).