Stem Cells - VCU Massey Cancer Center
advertisement
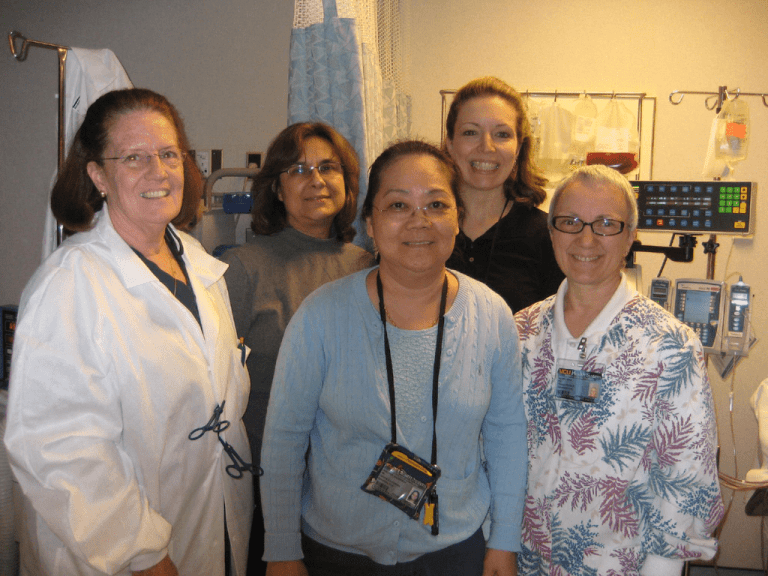
1 WHO ARE WE AND WHAT DO WE DO? 2 • Pathology Department/BMT • Transfusion Medicine • Medical Director – Dr. Susan Roseff • Asst. Medical Director – Dr. K Sanford • Jenni Anderson RN, HP(ASCP) • Susan Walker RN • Monica Utley RN • Louise Watlington RN • Renee King RN 3 Accreditation AABB CAP FDA FACT JACHO 4 What is Apheresis • Greek Word meaning to remove or separate. 5 6 Bone Marrow : Function •Production of red blood cells, white cells and platelets •170 billion red cells/day •70 billion granulocytes/day(neutrophils, eosinophils, • basophils) •175 billion platelets/day •Capable of 5-10 fold increase in production 7 Stem Cells: What are they? Life begins with stem cells from a fertilized egg. First as unspecialized cells that become specialized cells. Embryonic stem cells Fetal stem Cells Umbilical Cord stem cells Adult stem cells 8 • Vast majority of cells in the body are differentiated meaning they have taken on specialized properties and functions and have lost their ability to generate cells of other types e.g. skin, lungs, heart, bones. • There is another type of cells that are less differentiated and can give rise to other cell types and these are the stem cells. 9 Hematopeotic Stem Cells Capable of self renewal and production of a defined set of differentiated progenitor cells. Progenitor cells are multipotent with no capacity of self-renewal which differentiate and proliferate according to their pre-programmed destiny – Common Myeloid Progenitor Common Lymphoid Progenitor Megakaryocyte / Erythrocyte Progenitor 10 Stem Cells Marker •A CD34+ cell is a cell which had the CD34 antigen on its •surface. •This antigen is present on stem cells and colony •forming units as well as some other cell types. •This cell antigen is used as a surrogate marker for •multipotent stem cells. •“CD” refers to the “Cluster Designation” group of the •surface antigen. 11 CD34+ Multipotential Stem Cell Committed Stem Cells BFU-E CFU-Meg CFU-GM CFU-G CFU-Ba CFU-Eo CFU-E CFU-Ms CFU-B CFU-T CFU-M CD4/CD8 B T Lymphocytes 12 PBSC Collection: When to Begin ? I see lots of CD-34 cells in your future… 13 G-CSF Stimulation: How does it work ? Less than 0.01% in peripheral without stimulation. G-CSF Stem Cells 14 Effects of Mozobil 15 How do we mobilize stem cells ? G-CSF CD-34 Growth factor only 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Growth factor + post chemo (Cy+ G-CSF) G-CSF CY CD-34 1 1 2 3 4 5 6 7 8 2 3 4 5 9 10 11 12 13 14 15 16 17 18 19 Chemo +Growth factor 16 Requirements for Apheresis Venous access • Peripheral access? Smallest needle #17G • DL Dialysis type catheter (Permacath) • Dialysis shunts • Femoral only for limited number of procedures (peds) • #8F and above for DL catheter for peds 17 Central Line Catheter 18 19 Centrifuge 20 21 Platelets (1040) Lympocytes (1050-1061) Buffy Coat Monocytes (1065 - 1069) Granulocyte (1087 - 1092) RBC 22 23 Chasing after Stem Cells 24 25 PBSCC: Procedure 26 How long does the procedure take? • Large Volume (24L) collection. • On a good day 4.5 hrs collection. • On a not so good day maybe 5 - 6 hrs. • On a bad day longer than 6 hrs. • Pediatric patients usually take about 2.5hrs if we • have good access but may take a whole day • for line placement. 27 Donor Lymphocyte Infusion (DLI) •DLI is the infusion of Donor Lymphocytes from the donor of stem cell graft to the graft recipient for the purpose of combating or preventing relapse of the cancer the patient is receiving treatment for. •Can collect upfront during SC harvest and use part of the stem cells for DLI •Recruit donor at later date for collection. 28 Goal for collection? How do we know when we have enough cells?? •BMT sends orders to Apheresis to collect depending on what kind of transplant protocol. •Single auto transplant usually requires 5x10E6 CD34+/Kg •Tandem transplant 8 - 10 x 10E6 CD34+/kg. •Collections may take from 1 to 10 days to collect depending on peripheral CD34+ cell ct. •Collection starts when peripheral CD34+ cells is >10 - 15/uL 29 Side Effects during stem cell collection •G-CSF side effects: headache, flu like symptoms, bone pain. •Machine is primed with Saline and ACD-A (Citrate) •Citrate is used to prevent clotting. •Citrate ratio:10 -14 :1 depending on plt ct. •Citrate binds free ionized calcium to prevent blood from •clotting. •Citrate toxicity quite common with perioral tingling, •peripheral/facial tingling, nausea, vomiting. •May progress to prolong Q-T interval • Tetany if not corrected. 30 QA Management •Very much a part of Apheresis SC collection •Donor Screening/Eligibility •Donor safety •Product Collection - culture, viability, product purity •Pt Engraftment and Outcome, ongoing audits •Lots of long meetings with BMT 31 What is photopheresis • Photopheresis (ECP) is an immunomodulating therapy treatment using the Therakos UVR® XTS instruments. • First introduced for the treatment of CTCL which is only FDA approved treatment. 32 Clinical Indications for ECP • Malignancy: CTCL (ASFA Category I) • Graft Vs Host Disease • Organ Rejection • Autoimmune disorders: Systemic Sclerosis Rheumatoid Arthritis SLE Crohn’s Disease 33 GVHD • Can be acute and chronic • Acute GVHD occurs 10-18% of patients who receive allo HSCT despite prevention with immunosuppressive agents usually happens within 100days. • Happens when donor T cells recognize recipient HLA molecules as non self and react against those tissues. • Caveat is that it is these donor T-lymph's that facilitate engraftment in the marrow as well as the graft versus leukemia effect. 34 Technical Aspects • First phase: Leukopheresis Harvesting of WC 3 to 6 cycles depending on extracorporeal volume tolerance by patients. Buffy coat mononuclear cells diverted into a temporary collection bag. Pt’s RBCs and plasma returned to pt End product of 260cc to over 300cc. 35 36 37 Buffy coat 38 39 Technical Aspects of Photoactivation Phase • Buffy coat cells incubated with 8-Mop and pumped through photoactivation chamber and exposed to UVA radiation 8-Methoxypsoralen (UVADEX) induce mitochondrial damage of T cells. 40 Photopheresis • Photopheresis induces apoptosis of the treated. • Reinfused apoptotic cells generate tolerogenic antigen presenting cells which helps restore the immune system. • Cross linking of double strand DNA of T cells help disrupt their proliferation 41 Treatment schedule for photophersis • In acute GVHD who are refractory to steroid and anti rejection meds we may be asked to do 3x weekly for 8 to 12 weeks then taper to 2x weekly or every other week. • Chronic GVHD may start with 2x every other week for 3 to 6 months then taper. • cGVHD can last for years. Some patients stay on photopheresis for a long time. • Last treatment to be discontinued. 42 43 • Many Thanks to Dr. Torloni • Dr. Susan Roseff • Apheresis nurses 44