Blood Vessels - BradyGreatPath

Blood Vessels
Blood Vessels: The Vascular System
Transport blood to the tissues and back
Carry blood away from the heart
Arteries
Arterioles
Arterioles
Exchanges between tissues and blood
Capillary beds
Return blood toward the heart
Venules
Veins
Venules
Cross-section of Artery & Vein
Assume you are viewing a blood vessel under the microscope. It has a lopsided lumen, relatively thick externa, and a relatively thin media. Which kind of blood vessel is this?
Figure 11.9a
Tunic
Name and describe from the inside out the three tunics making up the walls of arteries, and veins, and give the most important function of each
Tunica intima
Tunica media
Tunica externa
Description
A single layer of squamous epithelium
A middle layer, consisting of smooth muscle and connective tissue
(primarily elastic fibers)
The outermost layer, made of fibrous connective tissue
Function provides a smooth, friction-reducing lining for the vessel.
The smooth muscle is activated by the sympathetic nervous system when vasoconstriction (and increases in blood pressure) is desired.
The elastic fibers provide for stretching and then passive recoil of vessels close to the heart, which are subjected to pressure fluctuations basically a protective and supporting layer
Blood Vessels: The Vascular System
Figure 11.9b
Why are artery walls so much thicker than those of corresponding veins?
Arteries are much closer to the pumping action of the heart and must be able to withstand the pressure fluctuations at such locations. Veins, on the distal side of the capillary beds of the tissues, are essentially low-pressure vessels that need less strength/support/ elasticity than do arteries.
Figure 11.9a
Skeletal Muscles and Valves
Name three factors that are important in promoting venous return.
1. The presence of valves ,
2. the milking action of skeletal muscles against the veins as the muscles contract,
3. the respiratory pump (pressure changes in the thorax during breathing)
Figure 11.10
Breathing in pulls blood into right atrium from vena cava
the “thoracic pump” which generates negative pressure in the lungs during inhalation causing blood to rush through the vena cava and right heart filling the dense
The thoracic pump draws blood from the extremities on inhalation and sends blood throughout the body on exhalation
Arteries are often described as vessels that carry oxygen-rich blood, and veins are said to carry oxygen –poor (carbon dioxide-rich) blood. Name two sets of exceptions to this rule that were discussed in this chapter.
Pulmonary arteries carry oxygen-poor blood and pulmonary veins carry oxygen-rich blood.
Umbilical arteries carry oxygen-poor blood from the fetus and the umbilical vein carries the most oxygen-rich blood to the fetus.
Arteries lack valves, but veins have them. How is the structural difference related to blood pressure?
Blood pressure in veins is much lower in arteries because veins are farther along in the circulation pathway. Veins need extra measures to force blood back to the heart.
Describe the structure of capillary walls
Capillary walls are essentially just the tunica intima (endothelium plus the basement membrane); thus, they are exceedingly thin
.
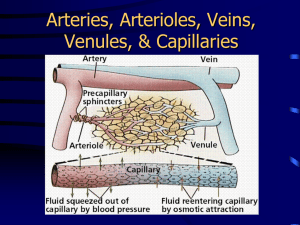
Capillary Beds
Capillary beds consist of two types of vessels
Vascular shunt—vessel directly connecting an arteriole to a venule
True capillaries—exchange vessels
Oxygen and nutrients cross to cells
Carbon dioxide and metabolic waste products cross into blood
How is the structure of capillaries related to their function in the body?
Capillary walls consist only of the innermost intima layer which is very thin. Capillaries are the exchange vessels between the and tissue, thus, thin walls are desirable
Left ventricle to ascending aorta
aortic arch
brachiocephalic artery
subclavian artery
axillary artery
brachial artery
radial (or ulnar) artery
capillary network of wrist
radial (or ulnar) vein
brachial vein
axillary vein
subclavian vein
right brachiocephalic vein
superior vena cava
right atrium of the heart.
Figure 11.12
Left ventricle ascending aorta aortic arch descending aorta right common iliac artery external iliac artery femoral artery popliteal artery anterior tibial artery dorsalis pedis artery
capillary network
anterior tibial vein popliteal vein femoral vein external iliac vein common iliac vein inferior vena cava right atrium of the heart.
Figure 11.12
In what part of the body are the femoral, popliteal, and arcuate arteries found
?
Lower Limb
In what part of the body are the axillary, cephalic, and basilic arteries found?
Upper Limb
What is the function of the hepatic portal circulation?
In what way is a portal circulation a “strange” circulation?
The hepatic portal circulation carries nutrient-rich blood from the digestive viscera to the liver for processing before the blood enters the systemic circulation.
A portal circulation involves a capillary bed that is both fed and drained by veins; the usual circulation has a capillary bed that is fed by arteries and drained by veins.
Figure 11.16
Which vessel – the hepatic portal vein, hepatic vein, or hepatic artery- has the highest content of nutrients after a meal?
The hepatic portal vein carries nutrient-rich blood from the digestive viscera to the liver for processing before the blood enters the systemic circulation. The liver removes nutrients (and toxins) from blood.
Comparison of Blood Pressures in Different Vessels
Figure 11.19
Capillary Exchange
Substances exchanged due to concentration gradients
Oxygen and nutrients leave the blood
Carbon dioxide and other wastes leave the cells
Capillary Exchange:
Direct diffusion across plasma membranes
Endocytosis or exocytosis
Some capillaries have gaps (intercellular clefts)
Fenestrations (pores) of some capillaries
What is the different about the capillary exchanges seen in a capillary with fenestrations and intracellular clefts and the exchanges seen in a capillary lacking those modifications?
Intercellular clefts allow limited passage of solutes and fluid.
Fenestrated capillaries allow very free passage of small solutes and fluids.
Capillaries lacking these modifications are relatively impermeable.
Figure 11.22
Capillary Types
Continuous basement membrane is continuous and intercellular clefts are tight; these capillaries have the lowest permeability.;
Fenestrated perforations (fenestrae) in endothelium result in relatively
high permeability.
Discontinuous − large intercellular gaps and gaps in basement membrane result in extremely high permeability
Fluid Movements at Capillary Beds
Blood pressure forces fluid and solutes out of capillaries
Osmotic pressure draws fluid into capillaries
Blood pressure is higher than osmotic pressure at the arterial end of the capillary bed
Blood pressure is lower than osmotic pressure at the venous end of the capillary bed
Would you expect fluid to be entering or leaving the capillaries at the venous end of a capillary bed?
Arterial end of capillary bed:
Fluid leaving capillary
Venous end of capillary bed:
Fluid entering capillary
Figure 11.23
Explain why blood flow in arteries is pulsatile* and blood flow in veins is not.
Blood flow in arteries is pulsatile because it is under a greater amount of pressure compared to veins.
Arteries are located closer to the ventricles, so their walls must be capable of expanding and contracting under the changes in pressure when the ventricles contract.
When blood reaches the veins, the pressure is very low, and so instead of veins having a pulsatile ability to maintain pressure, they instead have valves to prevent backflow
*beating rhythmically; pulsating or throbbing
What is the relationship between cross-sectional area of a blood vessel and velocity (speed) of blood flow in that vessel?
The greater the cross-sectional area in a blood vessel, the faster that blood can flow through that vessel.
Smaller vessels, like capillaries, are only one cell thick in diameter, which slows down blood flow and allows nutrient and gas exchange to occur.
Which type of blood vessel is most important in regulating vascular resistance*, and how does it achieve this?
Arterioles are the blood vessels that are most important in regulating vascular resistance.
These vessels can constrict as a result of activity from the sympathetic nervous system, which alters blood pressure.
(Arterioles are enervated by the sympathetic nervous system. Sympathetic nerve fibers secrete norepinephrine to receptors on the smooth muscles of arterioles causing contraction and thus leads to vasoconstriction.)
Atherosclerosis in these vessels also causes narrowing due to plaque deposits, which also affects blood pressure
*Resistance of blood flow through blood vessels
In a fetus, the liver and lungs are almost entirely bypassed by blood.
Why is this? Name the vessel that bypasses the liver. Name two lung bypasses. Three vessels travel in the umbilical cord; which of these carries oxygen and nutrient rich blood.
In a fetus, both liver and lungs are nonfunctional (the liver relatively so).
The
ductus venosus
bypasses the liver.
The
ductus arteriosus
and the
foramen ovale
bypass the lungs.
The umbilical vein carries nutrient-rich and oxygenrich blood to the fetus through the umbilical cord.
Ductus venosus BYPASS LIVER
What is the ductus venosus, and what is its function?
The ductus venosus is the liver bypass in the fetus.
Since the mother’s liver is working for the fetus as well, the entire fetal liver need not be continuously suffused with blood.
Liver
Foramen ovale & Ductus arteriosus
BYPASS LUNGS
Umbilical Cord- contains three blood vessels: two arteries and one vein.
Umbilical vein- bright red = high oxygenation
Umbilical arteries – pink = low oxygenation
Define pulse.
Pulse:The alternate expansion and recoil of an artery that occur with each heartbeat.
Which artery is palpated at the wrist? A
At the groin? B
At the side of the neck? C
At the front of the ear? D
At the back of the knee? E
D
C
A
B
E
Define systolic and diastolic pressure.
Systolic pressure—pressure in the arteries at the peak of ventricular contraction
Diastolic pressure—pressure in the arteries when ventricles relax
Two elements define blood pressure – the cardiac output of the heart and the peripheral resistance, or friction, in the blood vessels.
Name two factors that increase cardiac output.
Name two factors that increase peripheral resistance.
Cardiac output is increased by
• increased venous return
• increased heart rate.
Peripheral resistance is increased by
• decreased diameter of the blood vessels
• increased blood viscosity.
Increased venous return
Increased blood viscosity
How does blood pressure change throughout the systemic circulatory pathway?
It decreases from heart to vena cavae
What is the effect of hemorrhage on blood pressure? Why?
Hemorrhage reduces blood pressure initially because blood volume drops.
..Then the heart begins to beat more rapidly as it tries to compensate.
However because blood loss reduces venous return, the heart beats weakly and inefficiently. In such cases, the sympathetic nervous system causes vasoconstriction to increase blood pressure so venous return increases and circulation can continue.
In which position – sitting, lying down, or standing- is the blood pressure normally highest? Lowest?
Blood pressure is normally highest in the recumbent position and lowest immediately after standing up ; however, the sympathetic nervous system quickly compensates in a healthy individual.
Very often an individual can become hypotensive after remaining still in the sitting position for an extended period.
When you stand, gravity causes blood to pool in your leg veins,
Both systolic BP and diastolic BP were significantly higher in the supine than in the sitting position.
reducing the amount of blood that returns to your heart. This causes your blood pressure to drop