ACOT short
advertisement

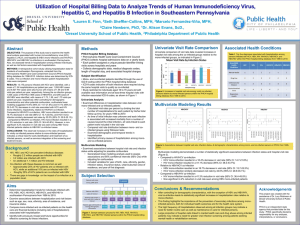
PHS GUIDELINE FOR REDUCING TRANSMISSION OF HUMAN IMMUNODEFICIENCY VIRUS, HEPATITIS B VIRUS AND HEPATITIS C VIRUS THROUGH SOLID ORGAN TRANSPLANTATION ACOT Conference Call February 28, 2012 Mandate • The National Organ Transplantation Act (1984 Pub.L. 98-507), which governs most aspects of organ transplantation in the United States, specifically requires the Secretary of the Department of Health and Human Services to contract with an Organ Procurement and Transplantation Network (OPTN) which, among other things, is required to: “adopt and use standards of quality for the acquisition and transportation of donated organs, including standards for preventing the acquisition of organs that are infected with the etiologic agent for acquired immune deficiency syndrome.” Current Reporting • In 2005, OPTN policy was revised to require OPOs and transplant centers to report potential donor-derived infections to the OPTN • Current standards by the Association of Organ Procurement Organization require deceased donor serum be maintained for 10 years following procurement of organs. • When an organ recipient is suspected of having a donor-derived infection, investigation ensues with testing of stored donor serum and recipient specimens in order to determine the infection source. Current Testing • OPTN policy requires deceased donor screening for anti-HIV, HBsAg, anti-HBc, and anti-HCV. • An FDA-licensed screening test is required for HIV, HBV and HCV • FDA approved tests include enzyme immunoassays that detect antibodies to the virus, antigen assays, and NAT. Magnitude of Problem • The estimated incidence of undetected viremia for normal-risk potential donors is 1 in 50,000 for HIV and 1 in 5,000 for HCV. For high-risk potential donors, the incidence of undetected viremia is 1 in 11,000 for HIV and 1 in 1,000 for HCV • A recent OPO survey found that the percentage of recovered organ donors who were reported as having “increased risk” behaviors varied among these organizations from a range of 2.3% to 26.1% of annual donor volume. • Of the 80 potential donor-derived disease transmissions reported to UNOS from 2005-2007, 30 cases were confirmed with HIV, HBV and HCV were among the top five most reported suspected donor-derived transmissions. Of note, further testing of stored donor specimens were negative using NAT in most cases. • Update to 1994 Public Health Service (PHS) Guidelines for Preventing Transmission of HIV through Transplantation of Human Tissue and Organs • The most significant changes involve: – expanding the guideline to include hepatitis B virus (HBV) and hepatitis C virus (HCV), in addition to human immunodeficiency virus (HIV); – utilizing factors known to be associated with increased likelihood of HIV, HBV or HCV to identify potential donors at increased risk for transmitting infection; – distinguishing between expected and unexpected transmission of HBV and HCV in goals for prevention; and – limiting the focus to solid organ transplants and vessel conduits recovered for organ transplant purposes. “This guideline was based on a targeted systematic review of the best available evidence on preventing transmission of HIV, HBV, and HCV through solid organ transplantation.” Proposed ACOT Recommendation • Although ACOT appreciates the efforts made by the CDC and PHS to minimize the risk of transmission of HIV, HBV and HCV through organ donation, the initial intent of the current document was to provide both evidence based and expert input into how best to implement viral screening into both living and deceased donor solid organ transplantation. Given the limitations of the current draft version, the ACOT recommends to the Secretary of HHS to direct the CDC and PHS to work together with the varied representatives of the transplant and organ donor communities to revise the draft to better address the concerns outlined in their responses.