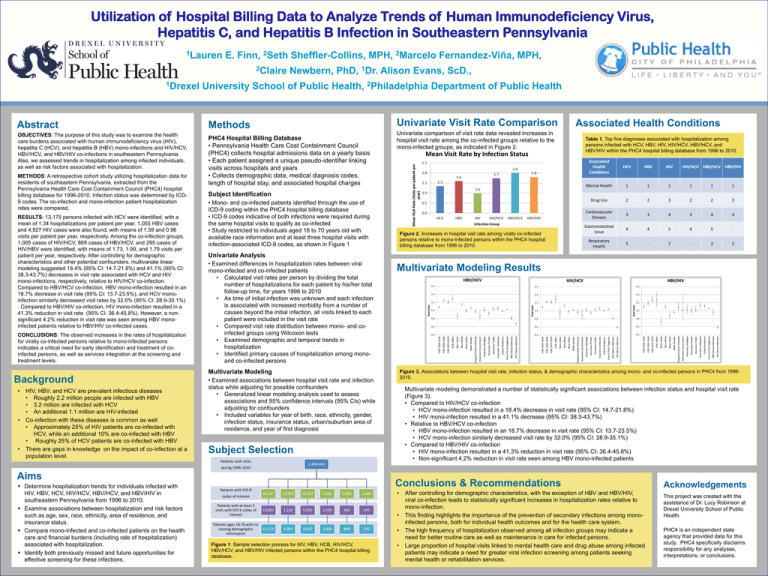
Utilization of Hospital Billing Data to Analyze Trends of Human Immunodeficiency Virus,
Hepatitis C, and Hepatitis B Infection in Southeastern Pennsylvania
1Lauren
E. Finn, 2Seth Sheffler-Collins, MPH, 2Marcelo Fernandez-Viña, MPH,
2Claire
1Drexel
Abstract
OBJECTIVES: The purpose of this study was to examine the health
care burdens associated with human immunodeficiency virus (HIV),
hepatitis C (HCV), and hepatitis B (HBV) mono-infections and HIV/HCV,
HBV/HCV, and HBV/HIV co-infections in southeastern Pennsylvania.
Also, we assessed trends in hospitalization among infected individuals,
as well as risk factors associated with hospitalization.
METHODS: A retrospective cohort study utilizing hospitalization data for
residents of southeastern Pennsylvania, extracted from the
Pennsylvania Health Care Cost Containment Council (PHC4) hospital
billing database for 1996-2010. Infection status was determined by ICD9 codes. The co-infection and mono-infection patient hospitalization
rates were compared.
RESULTS: 13,175 persons infected with HCV were identified, with a
mean of 1.34 hospitalizations per patient per year. 1,055 HBV cases
and 4,927 HIV cases were also found, with means of 1.59 and 0.98
visits per patient per year, respectively. Among the co-infection groups,
1,005 cases of HIV/HCV, 869 cases of HBV/HCV, and 295 cases of
HIV/HBV were identified, with means of 1.73, 1.99, and 1.79 visits per
patient per year, respectively. After controlling for demographic
characteristics and other potential confounders, multivariate linear
modeling suggested 18.4% (95% CI: 14.7-21.8%) and 41.1% (95% CI:
38.3-43.7%) decreases in visit rate associated with HCV and HIV
mono-infections, respectively, relative to HIV/HCV co-infection.
Compared to HBV/HCV co-infection, HBV mono-infection resulted in an
18.7% decrease in visit rate (95% CI: 13.7-23.5%), and HCV monoinfection similarly decreased visit rates by 32.0% (95% CI: 28.9-35.1%)
. Compared to HBV/HIV co-infection, HIV mono-infection resulted in a
41.3% reduction in visit rate (95% CI: 36.4-45.8%). However, a nonsignificant 4.2% reduction in visit rate was seen among HBV monoinfected patients relative to HBV/HIV co-infected cases.
CONCLUSIONS: The observed increases in the rates of hospitalization
for virally co-infected persons relative to mono-infected persons
indicates a critical need for early identification and treatment of coinfected persons, as well as services integration at the screening and
treatment levels.
Newbern, PhD,
1Dr.
Alison Evans, ScD.,
University School of Public Health, 2Philadelphia Department of Public Health
Methods
PHC4 Hospital Billing Database
• Pennsylvania Health Care Cost Containment Council
(PHC4) collects hospital admissions data on a yearly basis
• Each patient assigned a unique pseudo-identifier linking
visits across hospitals and years
• Collects demographic data, medical diagnosis codes,
length of hospital stay, and associated hospital charges
Univariate Visit Rate Comparison
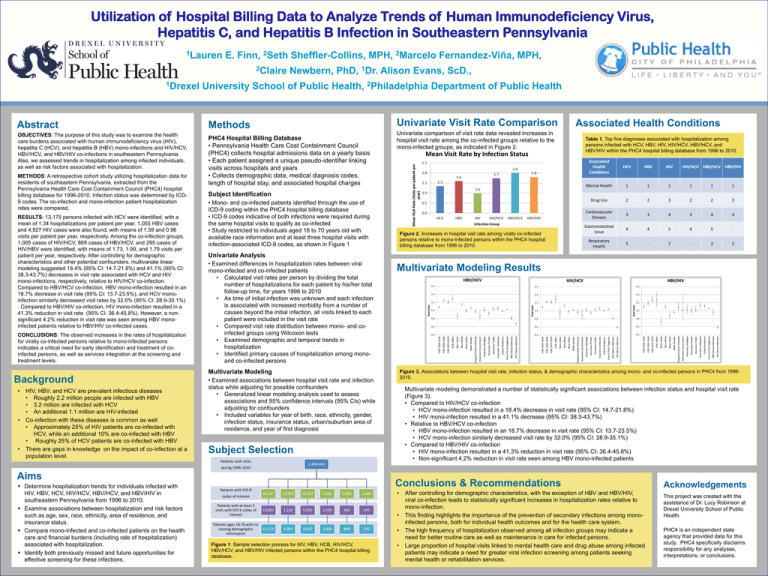
Univariate comparison of visit rate data revealed increases in
hospital visit rate among the co-infected groups relative to the
mono-infected groups, as indicated in Figure 2.
•
•
•
HIV, HBV, and HCV are prevalent infectious diseases
• Roughly 2.2 million people are infected with HBV
• 3.2 million are infected with HCV
• An additional 1.1 million are HIV-infected
Co-infection with these diseases is common as well
• Approximately 25% of HIV patients are co-infected with
HCV, while an additional 10% are co-infected with HBV
• Roughly 25% of HCV patients are co-infected with HBV
There are gaps in knowledge on the impact of co-infection at a
population level.
• Mono- and co-infected patients identified through the use of
ICD-9 coding within the PHC4 hospital billing database
• ICD-9 codes indicative of both infections were required during
the same hospital visits to qualify as co-infected
• Study restricted to individuals aged 18 to 70 years old with
available race information and at least three hospital visits with
infection-associated ICD-9 codes, as shown in Figure 1
Figure 2. Increases in hospital visit rate among virally co-infected
persons relative to mono-infected persons within the PHC4 hospital
billing database from 1996 to 2010.
Univariate Analysis
• Examined differences in hospitalization rates between viral
mono-infected and co-infected patients
• Calculated visit rates per person by dividing the total
number of hospitalizations for each patient by his/her total
follow-up time, for years 1996 to 2010
• As time of initial infection was unknown and each infection
is associated with increased morbidity from a number of
causes beyond the initial infection, all visits linked to each
patient were included in the visit rate
• Compared visit rate distribution between mono- and coinfected groups using Wilcoxon tests
• Examined demographic and temporal trends in
hospitalization
• Identified primary causes of hospitalization among monoand co-infected persons
Multivariate Modeling Results
Figure 3. Associations between hospital visit rate, infection status, & demographic characteristics among mono- and co-infected persons in PHC4 from 19962010.
• Examined associations between hospital visit rate and infection
status while adjusting for possible confounders
• Generalized linear modeling analysis used to assess
associations and 95% confidence intervals (95% CIs) while
adjusting for confounders
• Included variables for year of birth, race, ethnicity, gender,
infection status, insurance status, urban/suburban area of
residence, and year of first diagnosis
Multivariate modeling demonstrated a number of statistically significant associations between infection status and hospital visit rate
(Figure 3).
• Compared to HIV/HCV co-infection
• HCV mono-infection resulted in a 18.4% decrease in visit rate (95% CI: 14.7-21.8%)
• HIV mono-infection resulted in a 41.1% decrease (95% CI: 38.3-43.7%)
• Relative to HBV/HCV co-infection
• HBV mono-infection resulted in an 18.7% decrease in visit rate (95% CI: 13.7-23.5%)
• HCV mono-infection similarly decreased visit rate by 32.0% (95% CI: 28.9-35.1%)
• Compared to HBV/HIV co-infection
• HIV mono-infection resulted in a 41.3% reduction in visit rate (95% CI: 36.4-45.8%)
• Non-significant 4.2% reduction in visit rate seen among HBV mono-infected patients
Subject Selection
Aims
Determine hospitalization trends for individuals infected with
HIV, HBV, HCV, HIV/HCV, HBV/HCV, and HBV/HIV in
southeastern Pennsylvania from 1996 to 2010.
Examine associations between hospitalization and risk factors
such as age, sex, race, ethnicity, area of residence, and
insurance status.
Compare mono-infected and co-infected patients on the health
care and financial burdens (including rate of hospitalization)
associated with hospitalization.
Identify both previously missed and future opportunities for
effective screening for these infections.
Table 1. Top five diagnoses associated with hospitalization among
persons infected with HCV, HBV, HIV, HIV/HCV, HBV/HCV, and
HBV/HIV within the PHC4 hospital billing database from 1996 to 2010.
Subject Identification
Multivariate Modeling
Background
Associated Health Conditions
Conclusions & Recommendations
•
•
•
Figure 1. Sample selection process for HIV, HBV, HCB, HIV/HCV,
HBV/HCV, and HBV/HIV infected persons within the PHC4 hospital billing
database.
•
After controlling for demographic characteristics, with the exception of HBV and HBV/HIV,
viral co-infection leads to statistically significant increases in hospitalization rates relative to
mono-infection.
This finding highlights the importance of the prevention of secondary infections among monoinfected persons, both for individual health outcomes and for the health care system.
The high frequency of hospitalization observed among all infection groups may indicate a
need for better routine care as well as maintenance in care for infected persons.
Large proportion of hospital visits linked to mental health care and drug abuse among infected
patients may indicate a need for greater viral infection screening among patients seeking
mental health or rehabilitation services.
Acknowledgements
This project was created with the
assistance of Dr. Lucy Robinson at
Drexel University School of Public
Health.
PHC4 is an independent state
agency that provided data for this
study. PHC4 specifically disclaims
responsibility for any analyses,
interpretations, or conclusions.