The Radiation Oncology EHR of the Future
advertisement
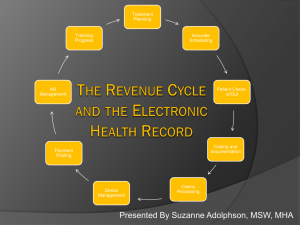
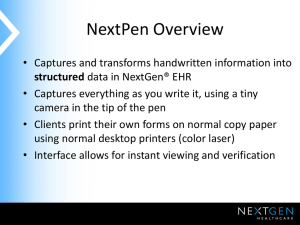
The Radiation Oncology EHR of the Future Joel W. Goldwein, MD Senior Vice President and Director Medical Affairs Elekta, Inc. August 6, 2010 Future Radiation Oncology EHR: Agenda • What’s the current state of the art? • What’s driving progress? • Where are we going? State of the Art: Radiation Oncology EHR • RT used in approx 50% of 1.4M US cancer patients • ~ 2,100 RT facilities in US – > 70% utilize dedicated information systems – Represents ~ 500,000 new RT patients/yr managed using RO EHR • RO highly EHR-dependent clinical specialty (V&R…) – Degree of EHR use highly variable • Two major EHR vendors (Elekta MOSAIQ, Varian Aria) – Well established / managed – Regulated QA systems support software development – Numerous interfaces to devices/machines, TPS, HIS, PACS, lab… – Largely standards-based (DICOM-RT, HL7, AJCC, CTC(AE)…) – IHE-RO participants (committed to interoperability) RO EHR Features (Elekta MOSAIQ®) • Clinical – – – – – – – V&R CPOE Comprehensive noting/charting TPS interface/integration Medical oncology support Rule-based workflow management Numerous interfaces (lab, HIS, treatment machines…) • Image Management (2D, 3D, 4D) – Import/export/manipulate – Treatment related image (IGRT) management – Oncology PACS Integration RO EHR Features (Elekta MOSAIQ®) • Practice Management/Administrative – – – – Patient and Resource Scheduling Charge Capture/Billing Kiosk patient check in Inter/intra-product communications • Research – – – – – – Data collection and reporting Data trending Outcome analyses support Graphical data exploration Clinical Trial management Interfaces out to Cancer Registry and RO data aggregation products Graphical Data Exploration Module RO EHR Environment • Architecture – PC Based • Desktop workstations, laptop carts, limited mobile devices – Client/Server (MS-SQL) • Workstations - five to hundreds • LAN or WAN (Citrix) • Device and imaging environment highly variable – Cadre or product mix innumerable (linacs, protons, orthovoltage, TomoTherapy, TPS, HIS…) – Workflow associated with evolving clinical trends • Some FDA regulated EHR components – MLC control systems, Image management components EHR Clinical Trial Support Features • TrialCheck® (Coalition of Cancer Cooperative Groups) – Determine patient eligibility for clinical trials active at your facility – Based on clinical criteria (age, disease, stage, performance status…) available in EHR • Trial data collection support – import/export assessment templates • DICOM-RT image export to cooperative groups (RTOG…) • Integrated National Comprehensive Cancer Network (NCCN) guidelines Clinical Trial Eligibility Determination Screen Web-centered Collaboration: Established Community of EHR Users • Shareable Reports • Sharable Document Templates • Sharable Care Plans • Listserver (independent) • Infrastructure for future expansion EHR Snapshots Patient Face Sheet (Chart Cover) EHR Snapshots Patient Assessments (Labs, Vital Signs…) EHR Snapshots Treatment setup image verification (2D) EHR Snapshots X-ray Volumetric Image Guided RT RO EHR: Current Status Summary • Widely deployed systems across entire specialty • Largely standards based • Device, HIS, TPS interconnectivity and interoperability comprehensive • Modern UI, RO image-enabled • Support clinical, research and administrative aspects of RO practice robust • Mature, established vendors with regulated & structured development control systems Seems like it’s all there! What’s next? How can we leverage today’s products to build the system of the future? Some Rad Onc EHR Drivers • Health Information Technology for Economic and Clinical Health Act (HITECH) • Meaningful use and ARRA certification ► $$$ • Rapidly emerging technologies (device, imaging, techniques, software…) – All expensive; proof of utility often limited – Associated workflows will require EHR support – Associated high costs implicate Comparative Effectiveness Research (CER) • Recent safety-related incidents – Incent development of “safer” EHR systems • Rising costs with potential diminishing reimbursement – Incents increased efficiency by improving workflow and the Human-Computer Interface Meaningful Use (HITECH) Ambulatory Provisions • Qualified Eligible Provider Requirements – Meet ~ 20 MU criteria AND use certified EHR system • e.g. - CPOE medications (e-prescribing), clinical rules engine (decision support), capture vital signs, provide patient EHR access, supply summary of care record… • Payout to qualified/eligible providers begin 2011 MEDICARE PAYMENT SCHEDULE Initial Qualifying Year Calendar Yr 2011 2011 2012 2013 2014 2015 2016 TOTAL $18,000 $12,000 $8,000 $4,000 $2,000 $44,000 2012 2013 2014 > 2015 $18,000 $12,000 $8,000 $4,000 $2,000 $44,000 $15,000 $12,000 $8,000 $4,000 $39,000 $12,000 $8,000 $4,000 $24,000 $0 $0 $0 Meaningful Use (HITECH) Effect on Future of RO EHR • Certification is current major Vendor focus • Expected Results Core Import/Export Immunization registry Public registry export Administrative import/export Administrative Appt Reminders – Acceleration of EHR system enhancements Demographics Vital Signs Lab e-prescribe CPOE Problem lists Discharge Pt. summary Follow-up & scheduling – Improvements in scope of (meaningful) use Drug interactions & Import export Smoking Care migration and transfer Allergies/Alerts Med reconciliation standards –Privacy Overall: Limited (but important) on ROSupport EHR and Security Vocabularyeffect Decision Authentication Encryption ICD-9/10; CPT Guidelines features, development, and end-user adoption Disclosure Compliance Audit SNOMED Already available or in progress Interlocks and Alerts Emerging technologies as RO EHR drivers: • Are we moving too quickly? • Will there ever be sufficient supportive evidence? • Can EHR systems help us obtain it? • Will EHR’s be able to accommodate ever changing workflow? RO: Fodder for Comparative Effectiveness Research Economic Scene In Health Reform, a Cancer Offers an Acid Test By DAVID LEONHARDT Published: July 7, 2009 “The prostate cancer test will determine whether President Obama and Congress put together a bill that begins to fix the fundamental problem with our medical system: the combination of soaring costs and mediocre results. If they don’t, the medical system will remain deeply troubled, no matter what other improvements they make.” [Radiation] Oncology: A CER Priority? • Cancer focus of 6 primary IOM CER topics • Direct US cancer costs $80 Billion • RO consumes approx. 10%; growing fast! – Burden likely to fall on us to provide evidence basis • A real-time registry capturing patterns-of-care data may represent part of the solution Distribution of the IOM's Recommended CER Priorities Iglehart J. N Engl J Med 2009;361:325-328 Radiation Oncology Data Registry • Pilot Program Background – Est. 10/2008 as derivative of more mature Med Onc data program • Aim – Demonstrate proof of concept for establishment of central RO data warehouse derived from live EHRs – Establish basis for CER…. – Reduce costs of data collection • Method – Leverage widely deployed RO EHRs – Aggregate de-identified data collected in EHRs in routine course of care – Extensible/scalable design Registry Architecture • Small program installed on local EHR PC • Scheduled service runs program at some regular interval • Program runs => De-identified dataset created • Dataset uploaded to central data warehouse • Dataset aggregated Registry RODA EHR Facility 1 EHR Facility 3 EHR Facility 5 EHR Facility 4 EHR Facility n EHR Facility 2 RO Registry Pilot Results ASTRO 2009 Analysis 18 RO participants 121,000 patient records, 108,000 patient treatments Data completeness (quality) Date of Diagnosis: 29% complete Overall Stage: 21% complete Assessment Successful, but quality issues need to be addressed HITECH/MU may incent quality improvements If scaled, could represent real-time model dataset for CER, advocacy, administrative and clinical research… Could serve as feed for higher-level multi-purpose registries and complement US Cancer Registry program RO Registry Multi-Purpose Model • Opportunities – Specialized emerging technologies registries (SBRT, Protons…) – CER registry – Safety (near-hit) database – caBIG Grid RO EHRs and Safety • RO info systems have incorporated safety features such as V&R for decades • Evidence suggests these features do indeed enhance safety* • Contemporary systems designed top-down to minimize hazards • This has not always been the case *Frass et al – IJROBP - 1998 RO Control Systems: Vehicles of “Safety” ? WIRED Nov ‘05 • 2 of 10 (and the only “deaths by software”) were RO-related – 1985 – Therac 25 Linear Accelerator • 5 deaths • Significant changes in way RO software developed – 2000 – Multidata TPS (Panama) • 8 deaths RO EHR Systems and Safety The Radiation Boom Radiation Therapy Offers New Cures, and Ways to do Harm By WALT BOGDANICH Published: January 24, 2010 NY State Records 2001-2008 – 621 events, 1,264 causes, 2 notable deaths • 46% - missed target • 41% - wrong dose • 8% - wrong patient # 352 252 174 133 60 24 19 Cause Flawed Q/A plan Human data entry/calculation error Wrong patient, wrong site Wedge or collimator misused Hardware malfunction Software bug Erroneous software override RO Safety Record Event Type Events per million RT courses* Any ~ 10,000 - 20,000 Errors w/ significant clinical consequences ~ 1,000 – 10,000 Errors w/ serious clinical consequences ~ 5 - 10 Lots of caveats (e.g. – under-dosing, under-reporting) • Most events ≠ serious injury • RT safe, but could/should always be safer [~ 1M RT courses yearly in US (IMV Report – 2007)] * Munro – BJR 2007 Why, in era of sophisticated EHRs, does this still happen? • RO Highly Complex! – Diseases varied – Processes fluid – Humans involved (both sides of table) – EHRs can’t anticipate it all • Failure Mode and Effect Analysis (FMEA) – 269 course process nodes – 127 high risk failure modes EVALUATION OF SAFETY IN A RADIATION ONCOLOGY SETTING USING FAILURE MODE AND EFFECTS ANALYSIS Simplified RO Workflow Illustrating the multitude of opportunities to manage IJROBP, the 2008 RO process ERIC C. FORD, PH.D.,* RAY GAUDETTE, M.S.,* LEE MYERS, PH.D.,* BRUCE VANDERVER, M.D., LILLY ENGINEER, DR.P.H., M.D., M.H.A., RICHARD ZELLARS, M.D.,* DANNY Y. SONG, M.D.,* JOHN WONG, PH.D.,* AND THEODORE L. DEWEESE, M.D.* Hazard Mitigation Training & Guess? Education • Hierarchy of effectiveness Rules & Policies Reminders & Checklists Simplification & standardization Automation & Computerization Forcing functions & Constraints (Interlocks) Mitigation Strategies The EHR Solution? Leverage Hazard Mitigation Strategies to Reinforce EHR Safety Increase dependence on most reliable hazard mitigation strategies Iterate! Less Automation Where human intervention is required…Reduce dependence Training & Education Rules & Policies Reminders & Checklists Simplification & standardization Human Intervention Automation & Computerization Forcing functions & Constraints (Interlocks) Safer System => Forcing Functions in Medicine: Interlocks, Timeouts and Checklists They work! Supplied throughout EHR, devices and applications Next generation EHR Roll your own! Graphical Workflow Design Toolkit Gamma Knife Treatment Console Checklist MOSAIQ Universal Timeout MOSAIQ Workflow Manager Incorporate customized checkpoints w/ optional interlocks and alerts at any point Special attention to any/all high risk hazard nodes in work flow Requires iteration via ongoing FMEA EVALUATION OF SAFETY IN A RADIATION ONCOLOGY SETTING USING FAILURE MODE AND EFFECTS ANALYSIS ERIC C. FORD, PH.D.,* RAY GAUDETTE, M.S.,* LEE MYERS, PH.D.,* BRUCE VANDERVER, M.D., LILLY ENGINEER, DR.P.H., M.D., M.H.A., RICHARD ZELLARS, M.D.,* DANNY Y. SONG, M.D.,* JOHN WONG, PH.D.,* AND THEODORE L. DEWEESE, M.D.* IJROBP, 2008 MOSAIQ Workflow Manager Process Change Prescription Check Modality Automatic Script Customer Defined Task Ask for More Data with User-Defined Form Create QCL Item To Verify Info, etc. The Human-EHR Interface: A few words • Pen/paper – hard to compete, but also hard to “computerize” • PC / keyboard / structured data entry – slow, awkward, interferes with MD-patient relationship – BUT, structured data necessary for true benefits of EHR • Dictation / voice recognition – Faster, easier, more natural – BUT, natural language processing that would provide for creation of structured data far off • A number of solutions are on the horizon The Human-EHR Interface: Teamwork! Software usability Improvements Mobile devices MOSAIQ EHR Hardware usability improvements Kiosks and PRO Interfaces Interfaces (Lab, HIS, Vitals…) Interfaces galore Digital pen & paper Dictation + Natural Language Processing What’s the Long Term Vision? EHRs as the Cornerstone • Remote Care Monitoring and Delivery – Driven by efficiency, cost containment, and Rx consistency requirements – Facilitated via EHR • Radiation Oncology “Medical Home”* – Our “processes” are far to diverse, uncontrolled and unstructured – Demands on our time will only increase – Patients will demand more control of their care *An approach to providing comprehensive evidence-based, guideline-directed care... that facilitates partnerships between patients and providers RO EHR Systems of the Future RO EHR systems are already (arguably) most sophisticated in medicine Managing complex tasks in an increasingly complicated environment The unique mix of technical and clinical specialists immersed in the explosion of advanced technologies will continue driving this trend…. Which will be great for our patients! The Radiation Oncology EHR of the Future Joel W. Goldwein, MD Senior Vice President and Director Medical Affairs Elekta, Inc. August 6, 2010