Anaesthesia Crisis Simulation
advertisement
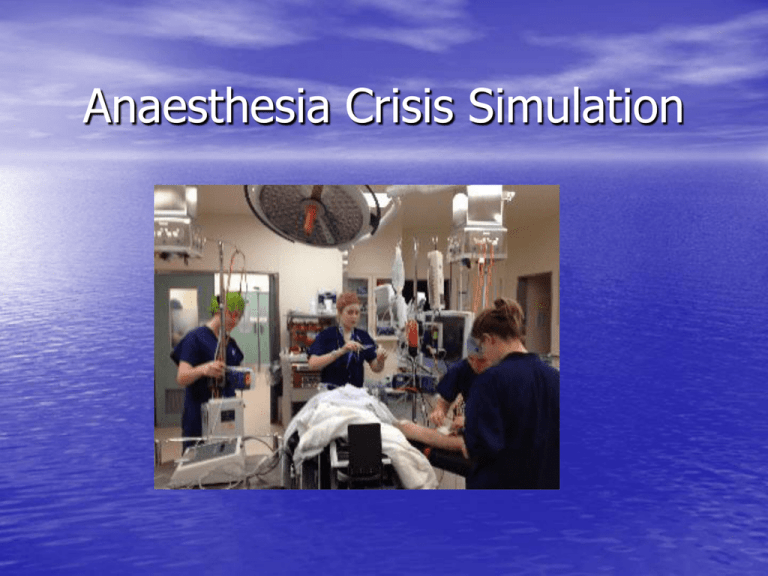
Anaesthesia Crisis Simulation Background • Anaesthesia early adoption SBME • Driven by Gaba, Emily Bromily • Similarities commercial airlines • Increased monitor/environmental fidelity • EMAC courses New Zealand • Both EMAC course providers in N Island • New anaesthetic registrar crisis course • More SBME for trainees near these centres But • Limited access for S island based Dr’s • Different equipment/environment • Lack of team based approach using local teams Christchurch Anaesthetics • Limited SBME despite demand PROMPT EMAC Course x1 in training CORE 7 EMST/APLS PATCH Ad hoc morning sessions The Problem • SBME effective • Significant simulation debriefing resources • Dose response relationship • Fidelity important to a point – buy in • Full simulation suite facilities expensive and not realistic for peripheral centres Solutions • 2 avenues 1) Collaborative approach with UoOSC 2) Development novel approach using equipment already available in the hospital at no cost. The “In situ” simulator • Clinical engineering calibration machines can be used to drive any monitor • This allows scenarios to be run “in situ” in the clinical environment Sp02 Sp02 • “False finger” to attach Sp02 probe • Dial up Sp02 and HR • Realistically changes over a number of seconds • Sometimes a little temperamental • Short period of flat line when changes made NIBP NIBP • Useful graduations 60/40, 80/50, 100/60, 120/80 etc • Y connector! MP450 ECG, IBP MP450 ECG, IBP • Allows adjustment HR and common rhythms. • Also invasive BP trace but fixed at 120/80 so limited utility. • Must attach to 5 lead ECG for all rhythms to be available The In situ OT set up Video Junior Trainee Crisis Sessions • 0700 coffee, muffins, Non threatening • 4 scenarios (anaphylaxis, MI VF arrest in PACU, Aspiration on LMA, Blocked ETT) • 4-6 trainees, 50% attended all. • Trainee tech • Guest “Volunteer” debriefer • Sign up sheet, evaluation survey and Post scenario resources provided on drop box supervised) other Seizure in PACU Failure to w ake in PACU MH Crisis MI LA Toxicity Anaphylaxis Burns Can't intubate, can't ventilate Endobronchial intubation SOB in PACU Cardiac arrest Massive Haemorrhage Bronchospasm Severe Trauma Severe Laryngospasm Failed intubation 0 2 4 6 1 Very Unconfident 2 3 4 5 Very confident Seizure in PACU Failure to wake in PACU MH Crisis MI LA Toxicity Anaphylaxis Burns Can't intubate, can't ventilate Endobronchial intubation SOB in PACU Cardiac arrest Massive Haemorrhage Bronchospasm Severe Trauma Severe Laryngospasm Failed intubation 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% These scenarios have been a valuable learning experience strongly disagree disagree neither agree nor disagree agree strongly agree Fidelity Fidelity of in OT set up 7 6 5 4 3 2 1 0 1 2 3 4 5 Fidelity (1: very unrealistic, 5 very realistic Fidelity Breakdown Patient fidelity (realism of mannekin, clinical findings compared to a real patient) Technical fidelity (similarity of machine, alarms, traces etc to normal workplace) 1 2 3 Environmental fidelity (similarity of environment eg. in theatre/drug trolley etc to normal workplace) 4 5 Scenario fidelity (clinical accuracy and realism of scenario) 0% 10 20 30 40 50 60 70 80 90 100 % % % % % % % % % % What were the strengths of the OT set up • More realistic, better prepared for real-life situation • Acting in real environment • same environment we spend the majority of our time in which makes how we might respond to the situation in real life more realistic and how we make use of the resources in that environment. • Familiar environment, with equipment that we use everyday. • It's where we work and where we would actually experience these events • Same environment as place of work. Realistic scenarios with added realism from use of usual monitors and anaesthetic machines. Weaknesses of in OT set up • Already identified, but would be useful having people • • • • • playing their usual roles, ie real nurses Difficult to hear lung sounds, other people in scenario should have a card of what they can / cannot offer to do having a scenario where when you do call for help and you gets heaps of willing assistants who may not be the most skilled/appropriate to assist in that particular situation and the subsequent distraction/stress this can provide and/or strains on communication when having to deal with that and the emergency at hand. Acting outside usual roles is unrealistic but necessary. Within limitations of mannikin (aka can't actually have real patients having cardiac arrest...) no real weaknesses Not using volatile is the only unrealistic aspect, but understandable. Issues • Clinical area limited availability scrupulous control of equipment • Set up time/ chasing collecting bits • Potential for unskilled debrief vulnerable participants • Dropbox Questions