Biology 20 – Respiratory System
advertisement

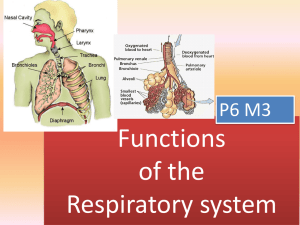
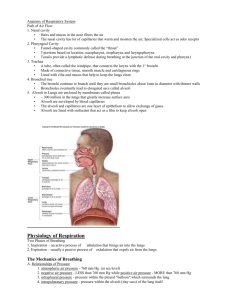
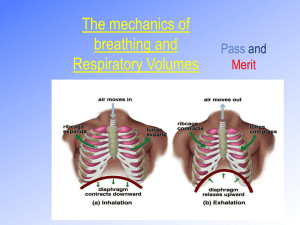
Biology 20 – Respiratory System • The air we breathe consists of nitrogen, carbon dioxide, trace gases and valuable oxygen vital for life. In humans, the only means we have of obtaining oxygen is through the lungs. Absence of oxygen for more than just a few minutes can result in death. Breathing • involves the movement of air between the lungs and the external environment. The processes involved in breathing include both inspiration and expiration. Breathing is not: Yawning - Stretching the facial muscles Hiccuping - Spasm of the diaphragm Respiration • involves all processes related to the exchange of oxygen and carbon dioxide, including breathing, gas exchange and cellular respiration. – External respiration – involves the exchange of oxygen and carbon dioxide between the air and the cells of the lungs. – Internal respiration – involves the exchange of oxygen and carbon dioxide between the blood and the tissue fluids. – Cellular respiration – involves the combustion of oxygen to produce ATP and carbon dioxide in the cells. Anatomy of the Respiratory System Respiratory System Anatomy • Nasal cavity – filters the air with the help of • • • cilia and mucous. It also moistens and warms the air before it goes to the lungs. Pharynx – opens from the nasal cavity and branches into two structures: Esophagus – muscular tube that moves food to the stomach. Trachea – the windpipe which is supported by C-shaped cartilaginous rings and covered with ciliated cells and mucous that act as a secondary filter. • Epiglottis – a flap of skin that • • covers the opening of the trachea to prevent food from entering the lungs while swallowing. Larynx – voice box, composed of 2 thin sheets of elastic ligaments that vibrate as air is forced out of them. These are also called the vocal cords and are protected by a thick band of cartilage called the Adam’s apple. Bronchi- are two tubes that branch from the trachea and carry air to the left and right lungs. • Bronchioles – smaller • branches off the bronchi that become progressively smaller until they reach the alveoli. Alveoli – air sacs in the lung where gas exchange occurs. Alveoli are covered with a slippery lipoprotein film called a surfactant that prevents the sacs from collapsing and sticking together. Gases diffuse in and out of the alveoli according to concentration gradients. • Pleural membranes – thin • membranes surrounding the outer surface of the lungs. They are filled with fluid to reduce friction between the lungs and the chest cavity during inhalation. Diaphragm – a large sheet of muscle that separates the organs of the thoracic cavity from those of the abdominal cavity. As the muscle contracts, the diaphragm flattens decreasing pressure inside the chest cavity, drawing air into the lungs. Relaxed, the muscle is dome-shaped. • Inter-costal muscles – • found between the ribs. As they contract, the ribs are pulled outward and upward, increasing the chest volume and contribute to inspiration. http://sprojects.mmi.mcgil l.ca/resp/anatomy.swf Breathing Movements • A pressure difference between the atmosphere and the chest cavity determine the movement of gases into and out of the lungs. Gases, like other substances, move from higher to lower concentration or from high pressure to low pressure. The diaphragm muscle and the intercostals muscles control and regulate pressure inside the chest in two ways: 1. When the muscle contracts, the diaphragm flattens and the ribcage lifts, increasing the chest volume, decreasing the pleural pressure. The result is air moving into the lungs during inspiration. 2. When the muscle relaxes, the diaphragm becomes dome shaped and the ribcage falls, decreasing the volume inside the chest, and increasing pleural pressure. The result is air moving out of the lungs during expiration. Habits of the Heart: The Lungs Breathing Movements Gas Exchange and Transport Dalton’s Law of Partial Pressure – each gas in a mixture exerts its own pressure, or partial pressure. The sum of the individual gas pressures add up to the total pressure. The partial pressure of oxygen and carbon dioxide varies in different parts of the respiratory system. • Pressure of oxygen in the air = 21 kPa • Pressure of oxygen in the alveoli = 13.3 kPa • Pressure of oxygen in the arteries = 12.6 kPa • Pressure of oxygen in the capillaries = 5.3 kPa • Transport of Gases in the Blood • oxygen is only slightly soluble in the blood (0.3mL / 100 mL), so it must be bound to hemoglobin to be transported in the blood. As oxyhemoglobin, the blood can carry 20 mL/100 mL of oxygen. The amount of oxygen that combines with hemoglobin depends on the partial pressures of oxygen in the blood and in the tissues. About 97% of all oxygen is carried by oxyhemoglobin, and the other 3% is carried in the plasma of the blood. • About 9% of the carbon dioxide is carried in the plasma and 27% is carried as carbaminohemoglobin (HbCO2), and 64% is carried as carbonic acid or bicarbonate. This reaction is catalyzed by the enzyme carbonic anhydrase. The reaction decreases the amount of carbon dioxide in the plasma, thus increasing the rate of diffusion of carbon dioxide from the cells to the blood. Once the blood is returned back to the lungs, the concentration of carbonic acid becomes very high, encouraging the diffusion of carbon dioxide out of the blood into the lungs. Ventilation – air flow in / out of the alveoli Perfusion – blood flow to the alveoli http://www.wisconline.com/objects/framz.asp?objID=AP2404 Animations Regulation of Breathing • Breathing is an autonomic function that is controlled by nerves from the medulla oblongata in the brain. Chemoreceptors detect the levels of carbon dioxide (acid) and oxygen in the blood and signal the brain to speed up or slow down breathing. 1. CO2 receptors – are activated when high levels of CO2 or H2CO3 are found in the blood. When these receptors are activated, they send nerve impulses to the rib s and diaphragm to increase breathing movements. CO2 + H2O - H2CO3 - H+ + HCO3+ 2. Oxygen receptors – are found in the carotid and aortic bodies in these arteries. If low levels of oxygen are detected, a message is sent to the medulla to increase breathing rate. Response to Exercise • Ventilation of the alveoli can increase up to 20 • • • • • times with heavy exercise. Muscles produce more CO2 and consume O2. The brain receives this information and increases breathing movements. Epinephrine is also released, increasing breathing. The lung exchanges more CO2 and O2. The kidney excretes excess acid from the blood. Breathing Disorders • Asthma – narrowing of/spasms of the muscles around the airways in the bronchioles that restricts oxygen flow. Asthma • Bronchitis – inflammation of the bronchioles, usually caused by a viral or bacterial infection, or by smoking. Lung Attack • Emphysema – is caused by chronic bronchitis until eventually, alveoli burst and scar tissue remains which irritate the bronchi. • Pheumothorax – is collection of air or gas in • • • the space surrounding the lungs, often caused by illness or traumatic injury. Air pressure within the pleural membranes is too high to allow air to be drawn in to the lungs. http://pneumothorax.org/pneumo.nsf/Pneumoth orax.swf Coughing - your trachea is covered in cilia (tiny hairs that prevent debris from entering the bronchioles. Smoking and exposure to other pollutants interferes with this process, and causes irritation and coughing. BioScope BioScope • Lung Cancer – the abnormal growth of cells in • the lung causing a tumour (a group of cancerous cells). http://www.davidberman.com/design/canceren.swf Spirometry – Measuring Lung Volume Lung capacity can be measured using a respirometer. Lung Capacity Measurements • Total Lung Capacity – the maximum volume • • • your lungs can stretch. Vital Capacity – the maximum amount of air that can be exhaled (after deep inhale) Tidal Volume (500 mL) – the amount of air inhaled and exhaled in a normal breath Inspiratory Reserve Volume (3000 mL) – is the amount of air that can be forcibly inhaled after a normal inhalation • Expiratory Reserve Volume (1500 mL) – is • • • the amount of air that can be forcibly exhaled after a normal exhalation Residual Volume (1000 mL)– the volume of air left in your lungs when all remaining air is exhaled. Inspiratory Capacity – the volume of air that can be forcible inhaled after a normal exhalation Functional Residual Capacity (2500 mL) – the total amount of air left in the lungs after a normal inhalation • Applet: review the static volumes • http://sprojects.mmi.mcgill.ca/resp/spirograph.swf