Anatomy of Respiratory System
advertisement

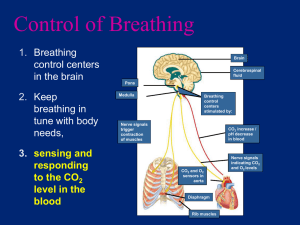
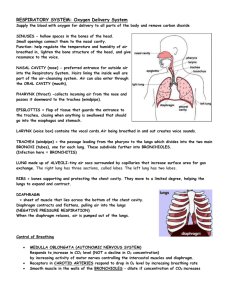
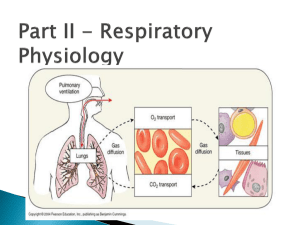
Anatomy of Respiratory System Path of Air Flow 1. Nasal cavity • Hairs and mucus in the nose filters the air • The nasal cavity has lot of capillaries that warm and moisten the air; Specialized cells act as odor recepto 2. Pharyngeal Cavity • Funnel-shaped cavity commonly called the “throat” • 3 portions based on location: nasopharynx, oropharynx and laryngopharynx • Tonsils provide a lymphatic defense during breathing at the junction of the oral cavity and pharynx) 3. Trachea • A tube, often called the windpipe, that connects the larynx with the 1° bronchi • Made of connective tissue, smooth muscle and cartilaginous rings • Lined with cilia and mucus that help to keep the lungs clean 4. Bronchial tree • The bronchi continue to branch until they are small bronchioles about 1mm in diameter with thinner walls • Bronchioles eventually lead to elongated sacs called alveoli 5. Alveoli in Lungs are enclosed by membranes called pleura • ~ 300 million in the lungs that greatly increase surface area • Alveoli are enveloped by blood capillaries • The alveoli and capillaries are one layer of epithelium to allow exchange of gases • Alveoli are lined with surfactant that act as a film to keep alveoli open Physiology of Respiration Two Phases of Breathing 1. Inspiration – an active process of inhalation that brings air into the lungs 2. Expiration – usually a passive process of exhalation that expels air from the lungs The Mechanics of Breathing A. Relationships of Pressure 1. atmospheric air pressure - 760 mm Hg (at sea level) 2. negative air pressure - LESS than 760 mm Hg while positive air pressure - MORE than 760 mm Hg 3. intrapleural pressure - pressure within the pleural "balloon" which surrounds the lung 4. intrapulmonary pressure - pressure within the alveoli (tiny sacs) of the lung itself B. Factors holding lungs AGAINST the thorax wall: 1. Surface tension holding the "visceral" and "parietal" pleura together 2. Intrapulmonary pressure ALWAYS slightly greater than intrapleural pressure by 4 mm Hg 3. Atmospheric pressure acting on the lungs Collapsed lung - hole in pleural "balloon" causes equalization of pressure and collapse of the lung II. Volume/Pressure & Inspiration/Expiration A. Boyle's Law on Volume/Pressure Relationships 1. Volume is INVERSELY proportional to Pressure a. INCREASE in Volume -> DECREASE in Pressure b. DECREASE in Volume -> INCREASE in Pressure Inspiration 1. diaphragm and intercostal muscle contracts, increasing thoracic cavity size. Volume Increases and pressure decreases 2. air rushes into lungs to fill alveoli Expiration 1. diaphragm and intercostal muscle relax, decreasing thoracic cavity size. Volume decreases and pressure increases 2. air pushed out of lungs 1. deep/forced inspirations - as during exercise and pulmonary disease 2. quiet expiration (exhalation) - simple elasticity of the lungs DECREASES volume -----> INCREASED pulmonary pressure -> movement of air out of the lungs 3. forced expiration - contraction of abdominal wall muscles (ie. obliques & transversus abdominus) further DECREASES volume beyond relaxed point ----> further INCREASE in pulmonary pressure -----> more air moves out Lung Compliance & Elasticity 1. fibrosis decreases lung compliance - the ease with which lungs can be expanded by muscle contraction of thorax 2. emphysema - decreases lung elasticity - the ease with which lungs can contract to their normal resting size (exhalation) 3. alveolar surface tension - liquid on surface of alveoli causes them to collapse to smallest size. Alveoli have a surfactant - lipoproteins that reduces surface tension on alveoli, allowing them to expand more easily Volumes, Capacities, and Function Tests A. Respiratory VOLUMES (20 yr old healthy male, 155 lbs.) 1. tidal volume (TV) - normal volume moving in/out (0.5 L) 2. inspiratory reserve volume (IRV) - volume inhaled AFTER normal tidal volume when asked to take deepest possible breath (2.1-3.2 L) 3. expiratory reserve volume (ERV) - volume exhaled AFTER normal tidal volume when asked to force out all air possible (1.0-2.0 L) 4. residual volume (RV) - air that remains in lungs even after totally forced exhalation (1.2 L) B. Respiratory CAPACITIES 1. inspiratory capacity (IC) = TV + IRV (MAXIMUM volume of air that can be inhaled) 2. functional residual capacity (FRC) = ERV + RV (all non-tidal volume expiration) 3. vital capacity (VC) = TV + IRV + ERV (TOTAL volume of air that can be moved) 4. total lung capacity (TLC) = TV + IRV + ERV + RV (the SUM of all volumes; about 6.0 L) C. Dead Space anatomical dead space - all areas where gas exchange does not occur (all but alveoli) Pulmonary Function Tests 1. spirometer - measures volume changes during breathing a. COPD - increased resistance to air flow (bronchitis or asthma) b. Restrictive disorders - decrease in Vital Capacity; lungs can’t inflate properly (TB, pulmonary fibrosis) Henry's Law of Gas Diffusion into Liquid. Henry's Law - a certain gas will diffuse INTO or OUT OF a liquid down its concentration gradient in proportion to its partial pressure Gases vary in their solubility - the ease with which a certain gas will "dissolve" into a liquid (like blood plasma) HIGHest solubility in plasma Carbon Dioxide, then Oxygen; LOWest solubility in plasma Nitrogen C. Hyperbaric (Above normal pressure) Conditions 1. Creates HIGH gradient for gas entry into the body 2. therapeutic - oxygen forced into blood during: carbon monoxide poisoning, circulatory shock, asphyxiation, gangrene, tetanus, etc. 3. harmful - SCUBA divers may suffer the "bends" when they rise too quickly and Nitrogen gas "comes out of solution" and forms bubbles in the blood Gas Exchange: Lungs, Blood, Tissues depends on Partial Pressure Gradients & Solubilities A. External Respiration (Air & Lungs) a. Oxygen: alveolar (104 mm) -------> blood (40 mm) Exchange is from aveoli to blood b. Carbon Dioxide: blood (45 mm) -------> alveolar (40 mm) exchange is from blood to alveoli (CO2 much more soluble than oxygen) B. Internal Respiration (Blood & Tissues) a. Oxygen: blood (104 mm) -------> tissues (40 mm) b. Carbon Dioxide: tissues (>45 mm) -------> blood (40 mm) Oxygen Transport in Blood: Hemoglobin: Association & Dissociation of Oxygen + Hemoglobin 1. oxyhemoglobin (HbO2) - oxygen molecule bound oxygen binds to heme 2. deoxyhemoglobin (HHb) - oxygen unbound H-Hb + O2 <========> HbO2 + H+ 3. Several factors regulate AFFINITY of O2 : Partial Pressure of O2, temperature, blood pH (acidity), Effects of Temperature HIGHER Temperature -----> Decreased Affinity (right) LOWER Temperature -----> Increased Affinity (left) Effects of pH (Acidity) 1. HIGHER pH--> Increased Affinity (left) 2. LOWER pH --> Decreased Affinity (right) "Bohr Effect" more Carbon Dioxide, lower pH, more O2 release Oxygen Transport Problems 1. hypoxia - below normal delivery of Oxygen 2. carbon monoxide poisoning - CO has greater Affinity than Oxygen or Carbon Dioxide Transport of Carbon Dioxide A. Dissolved in Blood Plasma (7-10%) B. Bound to Hemoglobin (20-30%) 1. carbaminohemoglobin - Car Diox binds to an amino acid on the polypeptide chains 2. Haldane Effect - the less oxygenated blood is, the more Carb Diox it can carry C. Bicarbonate Ion Form in Plasma (60-70%) Carbon Dioxide combines with water to form Bicarbonate CO2 + H2O <==> H2CO3 <==> H+ + HCO31. carbonic anhydrase - enzyme in RBCs that catalyzes this reaction in both directions a. tissues - catalyzes formation of Bicarbonate b. lungs - catalyzes formation of Carb Diox Carbon Dioxide Effects on Blood pH low pH -----> HCO3- binds to H+ high pH -----> H2CO3 releases H+ Neural Areas of Breathing in the Medulla stimulate the phrenic and intercostals nerves. Pons and Medulla Control of Breathing Rate & Depth 1. breathing rate - stimulation/inhibition of medulla; normal resting breath rate (12/minute) 2. breathing depth - activation of inspiration muscles 3. Hering-Breuer Reflex - stretch of visceral pleura that lungs have expanded (vagal nerve) D. Hypothalamic Control - emotion + pain to the medulla E. Cortex Controls (Voluntary Breathing) - can override medulla as during singing and talking Chemical Controls of Respiration A. Chemoreceptors (CO2, O2, H+) located in the medulla B. Carbon Dioxide is a powerful chemical regulator of breathing by increasing H+ (lowering pH) a. hypercapnia Carbon Dioxide increases ->DEPTH & RATE increase (hyperventilation) b. hypocapnia - abnormally low Carbon Dioxide levels which can be produced by excessive hyperventilation; breathing into paper bag increases blood Carbon Dioxide levels C. Oxygen Effects: large Ox decrease - stimulate increase ventilation hypoxic drive - chronic elevation of Carb Diox (due to disease) causes Oxygen levels to have greater effect on regulation of breathing D. pH Effects (H+ ion): acidosis - acid buildup (H+) in blood, leads to increased RATE and DEPTH (lactic acid) Exercise and Altitude Effects A. Exercise Effects (hyperpnea) - increase in DEPTH, not rate B. Altitude Effects O2 is lower at high altitude: Rates will increase. acclimatization - physiological adaptation to lower Oxygen content at higher altitude. Body "set-points" for Oxygen and Carb Diox will reset over a period of time Respiratory Disorders • Pneumonia – infection of the lungs with thick, fluid build up • Tuberculosis – bacterial infection that leads to tubercles (capsules) • Pulmonary fibrosis – lungs lose elasticity because fibrous connective tissue builds up in the lungs usually because of inhaled particles • Chronic Obstructive Pulmonary Disease (COPD) . almost all have smoking history, experience chronic "gasping" for air includes: • Emphysema – chronic, incurable disorder in which alveoli are damaged and thus the surface area for gas exchange is reduced, loss of elasticity of the lungs . Elastic Recoil is reduced so both airways are reduced and driving force behind expiration is reduced. • chronic bronchitis - mucus/inflammation of mucosa • Asthma – bronchial tree becomes irritated causing breathlessness, wheezing and coughing • Lung cancer – uncontrolled cell division in the lungs that is often caused by smoking and can lead to death. Treatment involves removing lobes of lungs called pneumonectormy.