Chapter 26
Lecture and
Animation Outline
To run the animations you must be in Slideshow View. Use
the buttons on the animation to play, pause, and turn
audio/text on or off.
Please Note: Once you have used any of the animation
functions (such as Play or Pause), you must first click on the
slide’s background before you can advance to the next slide.
See separate PowerPoint slides for all figures and
tables pre-inserted into PowerPoint without notes and
animations.
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chapter 26
Urinary System
26-2
26.1 Functions of the Urinary System
• Filtering of blood: involves three processesfiltration, reabsorption, secretion.
• Regulation of
– Blood volume
– Concentration of blood solutes: Na+, Cl-, K+, Ca2+,
HPO4-2
– pH of extracellular fluid: secrete H+
– Blood cell synthesis
• Synthesis of vitamin D
26-3
26.2 Kidney Anatomy and Histology
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
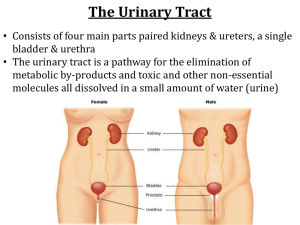
Kidney
Ureter
Urinary
bladder
Urethra
26-4
Location and External Anatomy of Kidneys
• Location
– Lie behind peritoneum
(retroperitoneal) on
posterior abdominal wall
on either side of vertebral
column
– Lumbar vertebrae and rib
cage partially protect
– Right kidney slightly lower
than left
• External Anatomy
– Renal capsule: fibrous connective
tissue. Surrounds each kidney
– Perirenal fat
• Engulfs renal capsule and acts as
cushioning
– Renal fascia: thin layer loose
connective tissue
• Anchors kidneys and surrounding
adipose to abdominal wall
– Hilum
• Renal artery and nerves enter and
renal vein and ureter exit kidneys
• Opens into renal sinus (cavity
filled with fat and loose connective
tissue)
26-5
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Liver
Spleen
Adrenal glands
Renal artery
Renal vein
Tenth rib
Left kidney
Right kidney
Inferior vena cava
Abdominal aorta
Ureters
Common iliac vein
Common iliac artery
Urinary bladder
Urethra
(a)
Body wall
Anterior view
Anterior
Parietal peritoneum
Renal vein
Peritoneal cavity
Renal artery
Liver
Inferior vena cava
Renal fascia
Abdominal aorta
Adipose tissue
Psoas major muscle
Renal capsule
Vertebra
Back muscle
(b)
Kidney
Posterior
Inferior view
26-6
Internal Anatomy of Kidneys
• Cortex: outer area
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Renal capsule
Cortex
Medulla
Artery and vein
in the renal sinus
Segmental artery
Renal sinus
(space)
Hilum (indentation)
Renal pyramid
Renal artery
Renal vein
Renal papilla
Minor calyx
Renal pelvis
Major calyx
Renal column
Medullary rays
(a)
Ureter
– Renal columns: part of
cortical tissue that extends into
medulla
• Medulla: inner area; surrounds
renal sinus
– Renal pyramids: cone-shaped.
Base is boundary between
cortex and medulla. Apex of
pyramid is renal papilla,
points toward sinus.
• Calyces
– Minor: papillae extend into
funnel of minor calyx
– Major: converge to form
pelvis
• Pelvis: enlarged chamber
formed by major calyces
• Ureter: exits at the hilum;
connects to urinary bladder
26-7
The Nephron
• Functional and histological unit
of the kidney
• Parts of the nephron:
Bowman’s capsule, proximal
tubule, loop of Henle
(nephronic loop), distal
tubule
• Urine continues from the
nephron to collecting ducts,
papillary ducts, minor
calyses, major calyses, and the
renal pelvis
• Collecting ducts, parts of the
loops of Henle, and papillary
ducts are in the renal medulla
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Glomerulus
Bowman
capsule
Renal
corpuscle
(cut)
Proximal convoluted
tubule
Nephron
Loop of
Henle
Distal
convoluted
tubule
Proximal
convoluted tubule
Distal
convoluted
tubule
Renal
corpuscle
Blood
supply
Juxtamedullary
nephrons have
loops of Henle that
extend deep into the
medulla.
Cortical nephrons
have loops of
Henle that do
not extend
deep into the
medulla.
Cortex
Thick segment
ascending limb
Loop of
Henle
Thin segment
ascending limb
Renal
pyramid of
the medulla
Thin segment
descending limb
Collecting ducts
Papillary
duct
Renal
papilla
To a minor calyx
26-8
Renal Corpuscle
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
• Bowman’s capsule:
cup-shaped structure
at the beginning of the
nephron
• Glomerulus: network
of capillaries. Blood
enters through afferent
arteriole, exits through
efferent arteriole.
Renal
corpuscle
Bowman
capsule
Glomerulus
Proximal
convoluted
tubule
Afferent
arteriole
Distal
convoluted
tubule
Efferent
arteriole
(a) The renal corpuscle consists of the Bowman
capsule and the glomerulus. The Bowman capsule
is the enlarged end of a nephron, which is indented
to form a double-walled chamber. The Bowman
capsule surrounds the glomerulus, which is a
network of capillaries. Blood flows from the afferent
arteriole into the glomerulus and leaves the
glomerulus through the efferent arteriole.
26-9
Histology of the Nephron
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Renal
corpuscle
Bowman
capsule
Glomerulus
(a) Juxtamedullary nephron
Proximal
convoluted
tubule
Distal
convoluted
tubule
• Proximal tubule: simple cuboidal
epithelium with many microvilli
• Loops of Henle
Nucleus
Mitochondrion
Microvilli
Basement membrane
(d) Distal convoluted tubule. The cells have
sparse microvilli and numerous
mitochondria, and they actively
reabsorb Na+, K+, and Cl–.
Ascending limb,
loop of Henle
Collecting duct
Invagination
• Distal tubule: shorter than
proximal tubule.
Descending limb,
loop of Henle
Mitochondrion
Basement membrane Tight junction
Nucleus
(b) Proximal convoluted tubule. The luminal
surface of the epithelial cells is lined with
numerous microvilli. The basal surface of
each cell rests on a basement membrane,
and each cell is bound to the adjacent cells
by tight junctions. The basal margin of each
epithelial cell has deep invaginations, and
numerous mitochondria are adjacent to the
basal membrane. Active reabsorption and
secretion are major functions.
Microvilli
• Collecting ducts: form where
many distal tubules come together.
Larger in diameter,. Form
medullary rays and lead to
papillary ducts
Mitochondrion Nucleus
Basement membrane
(e) Collecting duct. The cells have some
microvilli and numerous mitochondria, and
they actively reabsorb Na+, K+, and Cl–.
Papillaryduct
Mitochondrion
Microvilli
Nucleus Basement membrane
(c) Descending limb of the loop of Henle. The thin segment of the
descending limb is composed of simple squamous epithelial cells
that have microvilli and contain a relatively small number of mitochondria.
Water easily diffuses from the thin segment into the interstitial fluid.
26-10
Arteries and Veins of the Kidneys
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Arterial supply:
1. Renal arteries branch
from abdominal aorta
5. Interlobular
artery
4. Arcuate
artery
3. Interlobar
artery
2. Segmental
artery
11. Interlobular
vein
12. Arcuate
vein
13. Interlobar
vein
1. Renal
artery
14. Renal
vein
Medulla
Cortex
Ureter
Renal
pyramid
Renal
column
(a)
26-11
Arteries and Veins of the Kidneys
•
6.
7.
8.
9.
The part of the circulation
involved with urine formation
Afferent arterioles supply
blood to glomerulus
Glomerulus
Efferent arterioles exit the
renal corpuscle
Vasa recta: capillaries that
course into medulla along with
loops of Henle, then back toward
cortex (peritubular capillaries)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
8. Efferent
arteriole
Proximal
convoluted
tubule
Distal
convoluted
tubule
7. Glomerulus
6. Afferent
arteriole
Bowman
capsule
9. Peritubular
capillaries (blood
flows to the vasa
recta or directly to
the interlobular veins)
5. Interlobular
artery
Arcuate
artery
11. Interlobular
vein
Arcuate
vein
Ascending limb,
loop of Henle
Descending limb,
loop of Henle
10. Vasa recta
Collecting
duct
(b)
26-12
Arteries and Veins of the Kidneys
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
• Venous drainage
11. Renal veins
5. Interlobular
artery
4. Arcuate
artery
3. Interlobar
artery
2. Segmental
artery
11. Interlobular
vein
12. Arcuate
vein
13. Interlobar
vein
1. Renal
artery
14. Renal
vein
Medulla
Cortex
Ureter
(a)
Renal
pyramid
Renal
column
26-13
26.3 Urine Production
Nephrons considered functional units of the
kidney: smallest structural component capable
of producing urine
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Urine formation results from the following three processes:
1 Filtration
2
Tubular
reabsorption
3 Tubular
secretion
Filtration (blue arrow) is the movement
of materials across the filtration
membrane into the Bowman capsule
to form filtrate.
Solutes are reabsorbed (purple arrow)
across the wall of the nephron into the
interstitial fluid by transport processes,
such as active transport and
cotransport.
Water is reabsorbed (orange
arrow) across the wall of the nephron
by osmosis. Water and solutes pass
from the interstitial fluid into the
peritubular capillaries.
Peritubular capillaries
Interstitial fluid
2
3
1
Filtrate
Rest of the nephron
Bowman capsule
Glomerular capillaries
To interlobular
veins
Urine
Renal corpuscle
Efferent arteriole
Afferent arteriole
Solutes are secreted (green arrow)
across the wall of the nephron into the
filtrate.
26-14
Filtration
• Movement of fluid, derived from blood flowing through the
glomerulus, across filtration membrane
• Filtrate: water, small molecules, ions that can pass through
membrane
• Pressure difference forces filtrate across filtration membrane
• Glomerular filtration rate (GFR): amount of filtrate produced
each minute. 180 L/day
• Average urine production/day: 1-2 L. Most of filtrate must be
reabsorbed
26-15
Tubular Reabsorption: Overview
• Tubular reabsorption: occurs as filtrate flows through
the lumens of proximal tubule, loop of Henle, distal
tubule, and collecting ducts
• Results because of
–
–
–
–
–
Diffusion
Facilitated diffusion
Active transport
Symport
Osmosis
• Substances transported to interstitial fluid and
reabsorbed into peritubular capillaries: inorganic salts,
organic molecules, 99% of filtrate volume. These
substances return to general circulation through venous
26-16
system
Urine Production
• In Proximal convoluted
tubules
– Na+ and other substances
removed
– Water follows passively
– Filtrate volume reduced
• In descending limb of loop
of Henle
– Water exits passively, solute
enters
– Filtrate volume reduced 15%
• In ascending limb of loop of
Henle
– Na+, Cl-, K+ transported out of
filtrate
– Water remains
• In distal convoluted tubules
and collecting ducts
– Water movement out regulated
by ADH
• If absent, water not
reabsorbed and dilute urine
produced
• If ADH present, water moves
out, concentrated urine
produced
26-17
Urine Concentration Mechanism
• When large volume of water consumed
– Eliminate excess without losing large amounts of
electrolytes
– Response is that kidneys produce large volume of dilute
urine
• When drinking water not available
– Kidneys produce small volume of concentrated urine
– Removes waste and prevents rapid dehydration
• Mechanisms that create urine of variable concentration
– Maintenance of high concentration of solutes in medulla
– Countercurrent functions of loops of Henle
– Control of permeability of distal nephron to water
26-18
Urea
• Responsible for large part of
high osmolality in medulla
• Descending limbs of loops of
Henle permeable to urea;
urea diffuses into interstitial
fluid
• Ascending limbs and distal
tubules impermeable to urea
• Collecting ducts permeable to
urea; some diffuses out into
interstitial fluid
• Urea flows in a cycle
maintaining high urea
concentration in medulla
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Filtrate
flow
Descending
limb, loop of
Henle
Ascending
limb, loop
of Henle
Collecting
duct
Urea
Thin segment
Urea is
excreted in
the urine.
Urea contributes to
the interstitial fluid
solute concentration
and reenters the thin
segments of the loop
of Henle.
26-19
Urine Movement
• Hydrostatic pressure forces urine through
nephron
• Peristalsis moves urine through ureters from
region of renal pelvis to urinary bladder.
Occur from once every few seconds to once
every 2-3 minutes
– Parasympathetic stimulation: increase
frequency
– Sympathetic stimulation: decrease frequency
• Ureters enter bladder obliquely through
trigone. Pressure in bladder compresses
ureter and prevents backflow
26-20
Anatomy and Histology of Ureters and Bladder
• Ureters: bring urine from
renal pelvis to urinary
bladder.
• Urinary bladder: hollow
muscular container. In pelvic
cavity posterior to symphysis
pubis.
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Transitional
epithelium
(a)
Kidney
Ureter
Connective tissue
(lamina propria)
Smooth muscle layer
Connective tissue
(adventitia)
(b)
Parietal peritoneum
Urinary bladder
Opening of ureter
Trigone
Opening of urethra
Location of the
external urethral
sphincter
Transitional epithelium
Connective tissue
(lamina propria)
Smooth muscle layer
(detrusor muscle)
Connective tissue
(adventitia)
(c)
26-21
Anatomy and Histology of Urethra
• Male: extends from the inferior part of the urinary bladder
through the penis
• Female: shorter; opens into vestibule anterior to vaginal
opening
• Internal urinary sphincter: in males, elastic connective tissue
and smooth muscle keep semen from entering urinary bladder
during ejaculation
• External urinary sphincter: skeletal muscle surrounds urethra
as it extends through pelvic floor. Acts as a valve
26-22
Micturition Reflex
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Cerebrum
1 Urine in the urinary bladder stretches the
bladder wall.
2 Action potentials produced by stretch
receptors are carried along pelvic nerves
(green line) to the sacral region of the spinal
cord.
3 Action potentials are carried by
parasympathetic nerves (red line) to contract
the smooth muscles of the urinary bladder.
4 Ascending pathways carry an increased
frequency of action potentials up the spinal
cord to the pons and cerebrum when the
urinary bladder becomes stretched. This
increases the conscious urge to urinate.
5 Descending pathways carry action
potentials to the sacral region of the spinal
cord to tonically inhibit the micturition reflex,
preventing automatic urination when the
bladder is full. Descending pathways
facilitate the reflex when stretch of the
urinary bladder produces the conscious
urge to urinate. This reinforces the
micturition reflex.
6 The brain voluntarily controls the external
urethral sphincter through somatic motor
nerves (purple), causing the sphincter to
relax or constrict.
Pons
4
5
Ascending
pathways
Descending
path ways
2
Sacral region
of spinal cord
Pelvic
nerves
Parasympathetic
nerves
3
Ureter
Somatic
motor
nerves
1
6
Urinary
bladder
External urethral
sphincter
26-23
Please note that due to differing
operating systems, some animations
will not appear until the presentation is
viewed in Presentation Mode (Slide
Show view). You may see blank slides
in the “Normal” or “Slide Sorter” views.
All animations will appear after viewing
in Presentation Mode and playing each
animation. Most animations will require
the latest version of the Flash Player,
which is available at
http://get.adobe.com/flashplayer.
26-24
26.7 Effects of Aging
• Gradual decrease in size of kidneys, but only onethird of one kidney necessary for homeostasis
• Amount of blood flowing through gradually
decreases
• Number of glomeruli decrease and ability to
secrete and reabsorb decreases
• Ability to concentrate urine declines and kidney
becomes less responsive to ADH and aldosterone
• Reduced ability to participate in vitamin D
synthesis contributing to Ca2+ deficiency,
osteoporosis, and bone fractures
26-25