Reprocessing of Medical Devices (doc)
advertisement
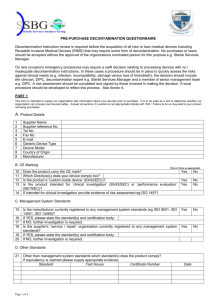
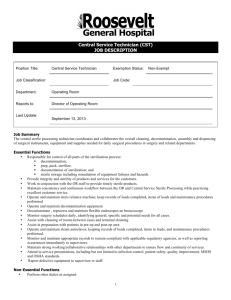
EAST CAROLINA UNIVERSITY INFECTION CONTROL POLICY Reprocessing of Medical Devices Date Originated: 2/26/08 Date Approved: 3/4/08 Page 1 of 4 Approved by: Date Reviewed: 3/1/11; 12/02/14; ___________________________ Vice Chancellor Health Sciences ___________________________ Director, Prospective Health ________________________________ Chairman, Infection Control Committee ____________________________ Infection Control Nurse 1 Reprocessing of Medical Devices I. Policy: It is the policy of East Carolina University and Brody School of Medicine to ensure patient clinical care items are decontaminated, disinfected, and/or sterilized according to the guidelines outlined in this policy and in compliance with all applicable regulatory agencies. I. Purpose: The purpose of this policy is to ensure decontamination, highlevel disinfection, and sterilization policies and procedures are standardized throughout the facilities in order to ensure the safety of patient care items. II. Procedures: A. Departments within the institution that process reusable medical devices/equipment within their department must develop written procedures for the components of reprocessing these items. B. The written procedure should be compliant with applicable standards and regulatory agencies. This includes but is not limited to: the method of sterilization or high-level disinfection, the physical facilities/work flow patterns, proper attire, and necessary training and educational requirements. C. The infection control practitioner will have oversight authority for the reprocessing of medical devices/equipment throughout ECU. D. General Requirements 1. Departments/Units must determine the feasibility of reprocessing reusable medical devices/equipment within their department utilizing the guidelines outlined in Appendix A. 2. Department /units that can comply with General Requirements may reprocess devices/equipment provided there are written procedures developed for the components of reprocessing performed. 3. Departments/Units that reprocess medical devices/equipment will adhere to the guide lines established in the following Infection Control Policies. Autoclave Use and Monitoring. Cleaning, Disinfection, and Sterilization of Patient Care Items Gluteraldehyde Usage Guidelines High level Disinfection of Endoscopic Equipment and Accessories Thermometer Use and Care Management of Clean, Soiled, and Sterile Supplies 2 Appendix A General Reprocessing Requirements I. Work Area Design, Work Flow Pattern, and Physical Facilities A. Work Areas: There must be designated areas for decontamination, preparation/packaging, high-level disinfection, sterilization, and storage. Infection Control must be involved in any of the planning, renovation or construction of existing space for these activities. B. Functional Work Flow Pattern: Functional work areas should be physically separated by walls or partitions to control contaminants generated during phases of reprocessing. Work flow and traffic patterns should be designed to flow from clean to soiled areas. C. Traffic Control: Traffic in all areas in which decontamination, preparation and packaging, sterilization processing, and sterile storage and distribution are performed should be restricted to facility personnel. Sterilizers should not be located in high traffic areas or near any potential sources of contamination such as cleaning/handwashing sinks or containers for the disposal of linen and trash. D. Physical Facilities: 1. Hand washing facilities: Hand washing facilities should be conveniently located in or near all decontamination, preparation, sterilization, and sterile storage areas. Hand washing sinks are not appropriate receptacles for the collection of soiled items. 2. Preparation and Assembly The area used for preparation and assembly of instruments to be sterilized should be physically separate from the decontamination area. If physical separation is not possible due to lack of space, at a minimum, plexiglass shields should separate the areas and each area thoroughly cleaned and decontaminated before it is used for clean preparation and assembly. 3. Housekeeping Procedures: Floors and horizontal work surfaces must be cleaned daily. Other surfaces, such as walls and storage shelves, should be cleaned on a regularly scheduled basis and more often if needed. Care should be taken to avoid the integrity of packaging during cleaning procedures. Special attention should be paid to the sequence of cleaning, to avoid transferring contaminants from dirty to clean areas. 3 II. Personnel Considerations 1. Qualifications a. All departments/units that perform reprocessing must have at least one supervisory individual who is prepared for this function by education, training, and experience. b. All personnel involved in reprocessing of reusable medical devices/equipment must, as a minimum, receive initial orientation, and on-the-job training, and continuing inservice education. 2. Personal Protective Equipment Requirements- Protective attire must provide suitable protection for the task being performed and must comply with OSHA regulations for the prevention of occupational exposure to bloodborne pathogens. a. Personnel who perform the decontamination process should wear: i. Heavy duty rubber or plastic gloves ii. Impervious shoe coverings iii. Water-proof apron/gown iv. Fluid impervious mask v. Eye protection 3. Health and Hygiene a. Personnel must comply with all applicable infection control policies and procedures. 4