reshaping care for older people and change plans
advertisement

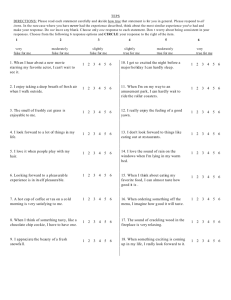
RESHAPING CARE FOR OLDER PEOPLE AND CHANGE PLANS Outer Hebrides Community Planning Partnership David Pigott JIT Associate Reshaping Care For Older People - Policy Goal: To optimise the independence and wellbeing of older people at home or in a homely setting Reshaping Care for Older People Commitments > Double the proportion of the total health and social care budget for older people that is spent on care at home > Build the capacity of third sector partners to help them do more to support the experience, assets and capabilities of older people > Introduce a Change Fund of in the region of £300 million over the period 2011/12 to 2014/15 > Shift resources to unpaid carers – at least 20% of fund Reshaping Care for Older People Commitments > Improve quality and productivity through reducing waste and unnecessary variation re emergency bed days > Reduce rates of emergency bed days used by those aged 75+ by a minimum of 20% by 2021 and at least 10% by 2014/15 > Ensure older people are not admitted directly to long term institutional care from an acute hospital > All older people over 75 years will be offered a telecare package in accordance with their assessed needs Shifting the balance….towards: Greater emphasis on preventative and anticipatory care A focus on recovery, rehabilitation and re-ablement Risk aware (not risk averse) Supporting engagement, self-worth and contributions (an asset based approach) Good information, advice and support to enable control and personalised care Good information, advice and support for unpaid carers Better alternatives to reduce bed days following emergency hospital admissions Integrated care and support and strong joint commissioning The Change Plans and Reshaping Care £80 million 2012/2013,circa £300 million over 4 years. A Programme for Change – 10 year Delivery Plan Updated Change Plans developed in the Spring Slow spend in year 1 Partnership planning process – Health, Local Government, third and independent sectors Development of joint commissioning strategies – to 2020 including funding and demographic projections for future years Consolidate 2011/12 actions and build on wide range of other innovative work underway , including Dementia From 2012/13 demonstrate at least 20% of spend dedicated to supporting carers Bridging finance to lever improvement across the entirety of older people’s spend in health and social care Meeting the challenges Demographic changes & finance Increased numbers requiring care & support within a tight financial envelope Status Quo will not suffice Shifts to anticipatory and preventative approaches Care based on principles of Co Production and effective partnership Change Fund leverage Change Fund=1%-2% Existing=98%-99% Health and social care expenditure Scottish population aged 65+ (2007/08 total=£4.5bn) Other Social Work Care Homes £0.2bn Emergency admissions £0.6bn £1.4bn Home Care £0.3bn FHS £0.4bn £0.4bn £0.4bn £0.8bn Other Hospital care Prescribing Community NATIONAL RESHAPING CARE PATHWAY (11/12 – mid-year review), (11/12 – plans) & (12/13) Preventative and Anticipatory Care (18%) (19%) (22%) Proactive Care and Support at Home (24%) (26%) (25%) Effective Care at Times of Transition (33%) (24%) (28%) Build social networks and opportunities for participation. Responsive and flexible home care. Reablement & Rehabilitation. Urgent triage to identify frail older people. Early diagnosis of dementia. Integrated Case/Care Management. Specialist clinical advice for community teams. Prevention of Falls and Fractures. Carer Support and Respite. NHS24, SAS and Out of Hours access ACPs. Early assessment and rehab in the appropriate specialist unit. Rapid access to equipment. Range of Intermediate Care alternatives to emergency admission. Information & Support for Self Management. Prediction of risk of recurrent admissions. Anticipatory Care Planning. Suitable, and varied, housing, build support and housing support. Timely adaptations, including housing adaptations and Telehealthcare. Hospital and Care Home(s) (19%) (23%) (16%) Prevention and treatment of delirium. Responsive and flexible palliative care. Effective and timely discharge home or transfer to intermediate care. Medicines Management. Medicine reconciliation and reviews. Access to range of housing options. Specialist clinical support for care homes. Enablers (6%) (7%) (8%) Outcomes-focussed assessment Co-production Technology/eHealth/Data Sharing Workforce Development/Skill Mix/Integrated Working OD and Improvement Support Information and Evaluation Commissioning and Integrated Resource Framework measuring shifts in balance of Care from institutions to home Partnerships need to know impact of actions Assurance also required for Ministerial Strategic Group Nationally available Outcome measures and indicators available for use Local Improvement measures where required Partnership Resource Use – Integrated Resource Framework Community Care Outcomes Framework Sustainability – Life after Change Fund Monitoring along the reshaping care pathway Prevention and Early Identification Learning from other programmes – e.g Dementia and associated demonstrator projects and research; Long Term Conditions; Carer Strategy Housing Strategy Community Capacity , Co-production & information investment Social Networks Prevention of falls Prediction of risk – SPARRA – Primary Care Anticipatory Care Planning Core Improvement Measures National Outcome measures and indicators Emergency admission bed day rates over 75s; delayed discharges data ; prevalence rates for diagnosis of dementia; % 65+ who live in housing rather than care home/hospital % time in last 6 months of life spent at home or in community setting; user and carer experiences Local Improvement Measures Anticipatory and preventative Proportion of over 75s at home with anticipatory care plan shared with out of hours staff; Waiting time between request for adaptation, assessment of need and delivery ; Proportion of over 75s with telecare; reduction in support required after reablement ; respite care per 1000 pop ; Acute demand and effective flow in Acute Care rates of 65+ to A&E after fall; proportion frail emergency admissions access to geriatric assessment within 24 hrs ; Long Term Residential Care level of admission of new entrants from home; hospital; after intermediate care ; graduate from emergency respite Partnership Resource Use Integrated Resource Framework data will be particularly useful Per Capita weighted cost of accumulated bed days lost to delayed discharge Cost of emergency bed days for over 75s per 1000 population A measure of balance of care split between spend on institutional and community based care Supporting Learning and Improvement Improvement Network established Regular network newsletters / Website Learning events and Web Ex sessions Gathering intelligence and disseminating examples of initiatives Specific development activities / events e.g. Joint Commissioning Strategies Involvement in development work on performance framework JIT link people to each partnership Community capacity and Co-production support Carers Issues support Other Areas of Direct Impact on Change Plans potential further integration of health and Social Care subject to legislation closer working between statutory partners to deliver better outcomes for all adults, bringing together health and social care resources, financial and operational Self Directed support Bill – partnerships to ensure SDS central to service options developed under change fund www.jitscotland.org.uk