Legal & Ethical Issues in Psychopathology
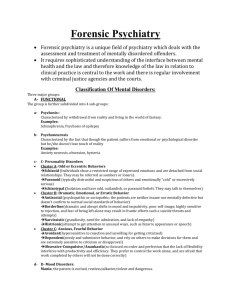
advertisement
Legal & Ethical Issues in Psychopathology Current Legal/Ethical Issues Legal Issues: Civil Commitment Criminal Commitment Duty to Warn Ethical Issues (in Treatment): Confidentiality Competence Dual Relationships Legal Issues Legal Issues Rights of patients vs. rights of public Few laws govern therapy Required to be competent To have a license Can use collection agencies if clients fail to pay Several unique legal issues with therapy Complex questions Burden therapist, state, others Civil Commitment Most hospitalizations are voluntary Voluntary is in best interest b/c can check out In some cases, patients are involuntarily hospitalized 1. 2. – Danger to oneself (suicidality) Danger to others (homocidality) Majority of commitments are male schizophrenics Civil Commitment Judge hears case & decides Hearing is requested by police, mental health provider Civil commitment must legally be lifted when patient is no longer dangerous Requirements protect patients - historically, anyone could have someone committed But, goals are re: danger, not helping The Right to Treatment Established 1972 by Wyatt v. Stickney Rationale for commitment = treatment Thus, if hospital is unwilling or unable to provide, patient can petition for commitment overruled Why suspend a patient’s rights unless there is a benefit? First attempt to have minimum criteria for mental health treatment The Right to Treatment Staffing levels, # of bathrooms, size of facility, variables that impact quality of life Rulings required states to provide facilities that met minimal requirements State provides most treatment for the severely and chronically mentally ill The Insanity Defense Based up on premise that people cannot be held responsible for crimes if they were unaware of the nature of their actions or were unable to control their actions We have free will to commit or not commit crime Legal insanity is a very narrow definition Psychological insanity: products of antecedents (a disorder is not something we choose) Insanity Defense Reform Act (1984) Made it more difficult to prove insanity Unable to appreciate wrongfulness as result of severe mental illness Defense now has burden of proof Previously, prosecution had to prove sanity Reduced advantages of pleading insanity Fixed minimum periods of incarceration Eliminated automatic release following reduction of danger Guilty But Mentally Ill Individual will be incarcerated, but acknowledges presence of mental illness Suggests that treatment is needed during incarceration Public Opinions of Insanity Pleas 90% of the public believes that: Public estimates of how many felony cases involve insanity pleas: 33% The insanity defense is used too much Lots of guilty people get to go free Actual number: <1% Public estimates of success: 50% Actual number: 25% Public Opinions of Insanity Pleas Public estimate of how many “insane” people are released: 50% Actual number: 15% (minor offenses that do not result in incarceration anyway) Public also tends to believe successful insanity pleas = short time in hospital They actually spend 50% longer in hospital then they would have in prison if guilty Competency to Stand Trial Is the person capable of understanding the charges and helping attorney to prepare the case? This is independent from sanity at the time of crime Trial is postponed; defendant is held for treatment Protects public from possible danger The Right to Refuse Treatment Can usually refuse treatment if desired Unless refusal is based on psychosis or delusions Before all commitments, independent evaluation is required (not connected to the hospital) Therapist’s Duty to Warn Tarasoff v. Regents of the U. of CA (1974, 1976) Therapists have a legal responsibility to warn potential victims when they may be at risk from a client 1969 Tatiana Tarasoff is murdered by a grad student who suggested, in therapy, that he was going to kill her Therapist informed police, who told grad student they were aware of his threats Grad student assured police he had no intentions of murder Therapist’s Duty to Warn Therapists are required to warn/protect potential victims By telling the police By committing the client By informing the potential victim Involves breaking a client’s confidentiality Ethical Issues Ethical Issues in Treatment 1. 2. 3. 4. 5. 6. Competence Integrity Professional & Scientific Responsibility Respect for People’s Rights & Dignity Concern for Others’ Welfare Social Responsibility Confidentiality Therapy is a protected relationship information is not shared without explicit permission Exceptions: Knowledge of child abuse Threats to others (Tarasoff) Threat to self Can consult with other therapists openly Competence Maintain the highest standards of competence Recognize & respect the limits of competence Provide only those services we are qualified to provide Competence is a combination of: education, training, experience Competence E.g. Conducting a neuropsyc assessment without training Be familiar with culture, gender, other differences & how those differences will effect one’s work Remain current in the field on research and professional information Record Keeping Maintain records of client contact to facilitate & document treatment Provide a basis for decisions Covers the therapist in case of legal action E.g. decisions regarding suicidality Records are often requested by insurance companies to determine if more services are needed Who is the Client? (Esp. Children) Psychologists may work with more than one person Ethics do not offer a clear line in this case Especially with children, who have parents & teachers, and other providers Avoid multiple roles Clarify roles if they are ambiguous Often ask parents for child’s confidentiality What if No Treatment Exists? Experimentation is required to further the field Clients should be informed of experimentation Clients also should be informed of other options that are established Often try experimental tx if an EST has been tried and failed (in clinical work) Design based on available science Dual Relationships When therapist/client relationship exists at the same time as another E.g. friend/friend or boss/employee Should therapists treat their friends? Should therapists treat/listen to their students? Some Practical Issues - Science vs. Pseudoscience The Widening Gap Between academic psychology & popular psychology Between research and general public knowledge Characteristics of Pseudoscience Overuse of ad hoc hypotheses to escape refutation Emphasis on confirmation, not refutation Absence of self-correction Reversed burden of proof Overreliance on anecdotal evidence Use of obscurantist language Absence of “connectivity” with other disciplines Pseudoscience in Psychopathology Explosion of unvalidated tx for trauma Use of demonstrably ineffective tx for autism Continued use of inadequate assessments Widespread use of herbal tx w/o testing Subliminal self-help tapes Explosion of self-help books and programs Suggestive techniques for memory recovery Why Should We Care? Why should we monitor the general public? Can’t they use whatever they want to buy? Techniques may be harmful to the public Consumers waste time & $ they could use in therapy Damage to our reputation & integrity Our ethical guidelines of social responsibility What Should Psychologists Do? Actively study & “debunk” pseudoscience Evaluate self-help materials Standardize training programs Popularize our findings & methods to the general public, convey our scientific excitement to outsiders & show the successful applications of it The general public is often unaware of what is proven, and what is not