Initial Response Team – Sunderland and South of Tyne
advertisement

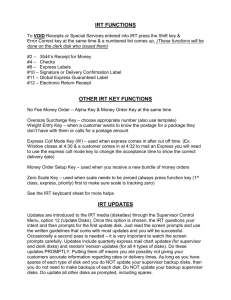
Initial Response Team Sunderland and South of Tyne Improving Access to Urgent Mental Health Services Dr Paul Brown- NTW Lead Consultant for Access, IRT/ CRHT David Hetherington- Senior Clinician- Sunderland IRT/ CRHT Rachel Winter- Sunderland IRT/ CRHT Clinical Lead Overview • • • • • Context Model Development Engagement and Commissioning IRT Evaluation Case Examples and Service User Feedback Service Model Request for Help Information & Advice Initial Response Initial evaluation regarding nature, risk, complexity and urgency of the problem More Intensive Packages of Care Hospital Signposting to principal service pathway for assessment and formulation Psychiatric Intensive Care Treatment Intensity Low Security Specialist Ward Crisis Beds PICU Environment Acute Ward Intermediate In the Community Low Security beds Intermediate Facility Challenging Crisis Bed Behaviour Acute Ward Mild severe non psychotic Very severe & complex nonpsychotic Psychosis Dementia Assessment Intensive Home Treatment At Home Intensive Home Home Etc. Challenging Behaviour Treatment Assessment Formulation & Treatment Planning Crisis Assessment Discharge Neuro disability Learning Disability Children & Young People Substance Misuse Scaffolding Medium Security Access? Access is the term used by NTW to describe the Initial Response to Urgent and Routine requests for help. Urgent Requests – Phase 1- (2012) Routine Requests – Phase 2- (2014) Integration with other routes of entry such as… • IAPT • Specialist Services • Social Care Demographics: North and South Population Geographic Area North of Tyne Northumberland North Tyneside Newcastle (18+) (18-65)* (18+) 225,100 254,979 (42% ) 127,560 (21% ) (37% ) 2000 miles sq 32 miles sq South of Tyne South Tyneside Sunderland (18+) (18+) Population 118,569 (26% ) 220,528 (47% ) Geographic Area 25 miles sq 53 miles sq 44 miles sq Gateshead (18-65)* 126,753 (27% ) Total 607,639 2076 miles sq Total 465,850 55 miles sq 133 miles sq Phase 1: The case for change Sunderland was chosen as the location for the development of a new access model following discussions with service users, carers, GPs and commissioners. •Clear issues with contacting the Crisis Team by phone as Triage saturated++ •Overnight and at peak demand times callers could wait hours for a return call from a clinician •No ready point of access for Older People or People with a significant Learning Disability seeking Urgent Advice/ Intervention •Fewer than 35% of referrals needed a Crisis Team Response •Most of the “inappropriate” calls required some form of advice/ signposting but at low risk/ acuity Engagement • Large scale events- Local Authority, GP’s, Commissioners, Service Users • Focussed Group Events- Service Users, GP’s, Staff Engagement- Commissioners • Sunderland PCT facilitated and supported Initial Engagement process • Recognised need for change • Supported 1st year (Pilot) through imaginative use of CQUIN • On basis of initial evaluation have commissioned ongoing service • Ongoing development of whole-system Initial Response Team South of Tyne and Wear Gateshead GH UCT ICTS Home Based Treatment Rapid Response 11 Nurses Information Collection & Routing Triage & Action South Tyneside REQUEST FOR HELP OPS Assessment Gatekeeping LD ST UCT ICTS Home Based Treatment Rapid 11 Response Nurses Triage & Action Sunderland OPS Assessment Gatekeeping LD SL UCT ICTS Home Based Treatment ROUTING Rapid 11 Response Nurses Triage & Action OPS Assessment Gatekeeping LD Phase 2 Model UCT IRT Urgent Rapid Response 11 Nurses Triage & Action Single Point of Referral ICTS Home Based Treatment OPS Assessment Gatekeeping LD Triage Team Noncomplex Clinical Diary Routine Complex Huddle Clinical Diary Phase 1: The Model •IRT to offer 24/7 Universal telephone access for requests for urgent help. •No restrictions on who could refer •Triage and Routing over the phone- (Mental Health and other local Services) •Face to Face Triage (Rapid Response) if clear plan cannot be determined over the phone •Seven Band 6 Nurses for Telephone and Rapid Response •Five Band 3 Nurses for call handling and Rapid Response •Use of digital dictation and 3G laptops for clinical documentation •Flexible interchangeable roles and rotation between Crisis Team and IRT roles dependant on demand. Phase 1: Benefits of IRT • Quick and efficient responses to requests for help • Effective routing to the correct services in and out of NTW • Flexible and collaborative working with newly configured UCT which will focus on the work for which it is commissioned • Reduction of clinician administration burden, and freeing time to care (mainly through adoption of digital dictation) • Improving personal and clinical outcomes for people in crisis with mental ill health by reducing harm and premature mortality, improving patient safety and patient experience Evaluation-IRT in numbers Typical weekly activity •1500+ •1000 •400 •50 •100 Incoming telephone calls Total Contacts Home-based Treatment contacts Crisis Assessments Rapid Responses …and growing •90% calls answered within 15 seconds •>98% within 3 minutes (Average=9 Seconds) •>80% rapid responses achieved in under one hour IRT Referrals (Q3 2013) Other includes: • Self Harm Team • Acute Care Trust • NTW Inpatient Ward • Ambulance • Consultant Psychiatrist • Residential Care Facility • Drug and Alcohol Services • IAPT • Member of Public • EDT • Probation Service Feedback Service User and Carer GP The service is responsive and friendly I felt listened to and was delighted Fantastic – a huge improvement!! You should have done it before Staff More manageable A lot happier Skills are valued Spend more time I cannot imagine where I would be today if you had not been there for me. I couldn’t have got this far without your help You do an amazing job! You listened and told me what to do Keep this very valuable service going You are all very dedicated, patient, compassionate people Wonderful support! Service User Feedback- Word Cloud Service User Narrative Feedback • “Its because of IRT that I haven’t self harmed in four months. Before, I would self harm two or three times a week and would end up in A&E, but knowing that they are there and knowing that I’m going to get the same positive response every time means that I have been able to listen to their advice and develop coping strategies. I’m much more hopeful about my future” Case Example 1- John- 31 • First contact from brother, family concerned ++ • “odd” ideas, becoming reclusive • Triage completed via Rapid Response (Face to Face) within one hour (after contact with John. • Engaged in period of home-treatmentreferred to EIP Case Example 2- Jenny 60 • • • • • Local Community Police Referral Jenny had been contacting them regularly Concern re mental health and self-neglect Rapid-Response to join police at property Crisis Assessment identified depression, alcohol dependence and social issues • Home Treatment • Joint work with social care Summary • IRT developed in a context of shared goals with commissioner and wider partners • IRT shown to vastly improve access & responsiveness with widely positive feedback • Next steps planned will look at incorporating all referrals and wider system