(CMHD): Slide set - National Collaborating Centre for Mental Health
advertisement
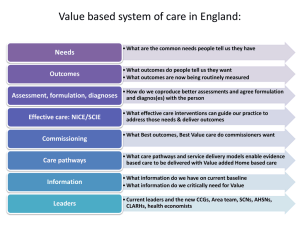
Common mental health disorders: identification and pathways to care Implementing NICE guidance within primary care 2011 NICE clinical guideline 123 What this presentation covers Scope Background Key recommendations for implementation Primary care costs avoided and benefits Discussion Find out more Scope The guideline aims to improve access to care and the identification and recognition of common mental health disorders, and provide advice on principles for local care pathways. Advice from existing NICE guidelines has been combined with new recommendations on access, assessment and local care pathways. Common mental health disorders include depression, panic disorder, generalised anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder and social anxiety disorder. Epidemiology • 15% of the population are affected by common mental health disorders • Women are 1.5 to 2.5 times more likely to experience depression than men • 34% of South Asian women have a common mental health disorder compared with 10% of South Asian men Background • Depression is a leading cause of disability – and it is projected to become the second most common cause of loss of disability-adjusted life years in the world • Only a small minority of people who experience anxiety disorders receive treatment • Recognition of anxiety disorders in primary care is particularly poor Abbreviations used CBT - cognitive behavioural therapy ERP - exposure and response prevention EMDR - eye movement desensitisation and reprocessing GAD - generalised anxiety disorder OCD - obsessive compulsive disorder IPT - interpersonal psychotherapy PTSD - post-traumatic stress disorder A full glossary of terms used in the guidance can be found alongside this slide set on the NICE website Key priorities for implementation Areas identified as key priorities for implementation: • Identification • Improving access to services • Developing local care pathways Identification: depression Be alert for possible depression, particularly in those with a past history or possible somatic symptoms of depression, or a chronic physical health problem Consider asking: • During the last month, have you often been bothered by feeling down, depressed or hopeless? • During the last month, have you often been bothered by having little interest or pleasure in doing things? Identification: anxiety 1 Be alert to possible anxiety disorders, particularly in those with a past history or possible somatic symptoms of an anxiety disorder, or who have experienced a recent traumatic event. Consider asking about feelings of anxiety and the ability to stop or control worry, using the GAD-2 scale. Identification: anxiety 2 Consider asking: Over the last two weeks, how often have you been bothered by the following problems? • Feeling nervous, anxious or on edge • Not being able to stop or control worrying GAD-2 is the first two questions of the GAD-7 scale The GAD-7 tool was developed by Drs. Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke and colleagues, with an educational grant from Pfizer Inc. Identification: anxiety 3 Score of 3 or more consider an anxiety disorder and follow the recommendations for assessment Score of less than 3 but you still have concerns that the person may have an anxiety disorder ask: Do you find yourself avoiding places or activities and does this cause you problems? N.B. The scoring of more or less than 3 applies to the use of the two GAD-2 questions Identification For significant communication difficulties, consider using the Distress Thermometer and/or asking a family member or carer about the person’s symptoms If identification questions indicate a common mental health disorder, a competent practitioner should perform a mental health assessment If this professional is not the person’s GP, inform the GP of the referral Assessment Consider using: • A diagnostic or problem identification tool, for example the Improving Access to Psychological Therapies (IAPT) screening prompts tool • A validated measure relevant to the disorder to inform assessment and support evaluation of interventions: - 9-item Patient Health Questionnaire (PHQ-9) - Hospital Anxiety and Depression Scale (HADS) - 7-item Generalized Anxiety Disorder scale (GAD-7) Ask directly about suicidal ideation and intent Assessment: core components Staff conducting assessments should be able to: - determine the nature, duration and severity of the presenting disorder - take into account symptom severity and associated functional impairment - identify appropriate treatment and referral options in line with relevant NICE guidance Consider factors that may affect the development, course and severity of a person’s presenting problem: - history of mental health disorder or chronic physical health - past experience and response to treatments - quality of interpersonal relationships - living conditions and social isolation Severity of common mental health disorders: definitions Mild relatively few core symptoms, a limited duration and little impact on day-to-day functioning Moderate all core symptoms of the disorder plus other related symptoms, duration beyond that required by minimum diagnostic criteria, and a clear impact on functioning Severe most or all symptoms of the disorder, often of long duration and with very marked impact on functioning Persistent subthreshold symptoms and associated functional impairment that do not meet full diagnostic criteria but have a substantial impact on a person’s life, and which are present for a significant period of time Stepped-care model CMHDs presentation and severity Recommended interventions Step 1 All disorders – known and suspected presentations All disorders: Identification, assessment, psychoeducation, active monitoring; referral for further assessment and interventions Step 2 Persistent subthreshold depressive symptoms or mild to moderate depression; GAD; mild to moderate panic disorder; mild to moderate OCD; PTSD (including mild to moderate) Depression GAD and panic disorder OCD PTSD All disorders – Support groups, educational and employment support services; referral for further assessment and interventions Step 3 Persistent subthreshold depressive symptoms; mild to moderate depression not responded to a lowintensity intervention; moderate or severe depression; GAD with functional impairment or has not responded to low-intensity intervention; moderate to severe panic disorder; OCD with moderate or severe functional impairment; PTSD Depression GAD Panic disorder OCD PTSD All disorders – Support groups, educational and employment support services; referral for further assessment and interventions Improving access to services Collaborate to develop local care pathways that: • support integrated delivery across primary and secondary care • have clear and explicit entry criteria • focus on entry and not exclusion criteria • have multiple means and points of access, including self-referral • have a designated lead to oversee care • promote access for people from socially excluded groups Developing local care pathways:1 Design local care pathways that promote a stepped-care model of integrated delivery to: • • • • • • • provide least intrusive, most effective interventions first have explicit criteria for different levels of intervention not base movement between levels on a single criteria monitor progress and outcomes minimise the need for transition between services establish clear access and entry points have designated staff responsible for coordination of care Developing local care pathways: 2 Develop protocols for communicating information: • • • • for service users about their care with other professionals (including GPs) between services within the pathway to services outside the pathway Robust systems should be in place to ensure routine reporting of outcomes Primary care costs avoided and benefits Due to variation in current practice, it is not possible to quantify the national cost impact of the NICE recommendations. The following areas may incur savings through drug costs avoided by meeting additional demand with treatments such as talking therapies. People with mild panic disorder. People with mild depression or anxiety or both. People who have mild moderate OCD. Estimated reduction in need - GP services and medications 60% Saving in GP visits and drug costs £ 471 per person Estimated reduction in need of medications 53% Saving in drug costs £202 per person Interventions for anxiety: potential costs Intervention Cost of intervention Identification and assessment Minimal Low-intensity psychological interventions (LIPI) £540 for 6 sessions or £45 per person based on a group of 12 Drug treatment From £189 to £449 High-intensity psychological interventions (HIPI) £1125 per person for 15 sessions Highly specialist treatment As shown for drug treatment & HIPI but combined. Inpatient episode £6496 Interventions for depression: potential costs Intervention stages Potential additional costs Principles for assessment, coordination of care and treatment choice It is estimated these recommendations will not incur any additional costs Step 2: recognised depression – persistent subthreshold depressive symptoms or mild to moderate depression Consideration should be given to the resourcing of group-based peer support (self-help) programmes Step 3: persistent subthreshold depressive symptoms or mild to moderate depression with inadequate response to initial interventions, and moderate and severe depression Any costs or savings resulting from these recommendations are likely to be based on local practice Discussion • How are diagnostic or problem identification tools used in primary care? What audit activity reviews their use? • How do our care pathways compare with the NICE guidance? • What methods are used to review service user treatment outcomes? • How can we address cases where there is persistent subthreshold CMHD symptoms? Find out more Visit www.nice.org.uk/guidance/CG123 for: • • • • • • • the guideline the quick reference guide ‘Understanding NICE guidance’ costing report and template baseline assessment Resource for primary care online educational tools Presenter notes The previous slide marks the end of the presentation; slides from this point on are for use by the presenter. For information, the stepped-care table on slide 16 contains action buttons that link to more detailed content (which is stored within slides 25-28). Action buttons only operate when the presentation is in slide show view. The presenter will need to click on a hyperlink to access the further detail. Feedback Did the implementation tool you accessed today meet your requirements, and will it help you to put the NICE guidance into practice? We value your opinion and are looking for ways to improve our tools. Please complete this short evaluation form The feedback survey can be accessed by right clicking your mouse over the hyperlink, and then selecting open hyperlink from the menu options Stepped care: depression Step 2 interventions Individual facilitated self-help Computerised CBT Structured physical activity Group-based peer support (self-help) programmes Non-directive counselling delivered at home* Antidepressants Self-help groups * for women during pregnancy or the postnatal period Step 3 interventions Back to stepped care table CBT IPT Behavioural activation Behavioural couples therapy Counselling Short-term psychodynamic psychotherapy Antidepressants Combined interventions Collaborative care (if chronic physical health problem) Befriending Rehabilitation programmes Self-help groups Stepped care: GAD and panic disorder Step 2 interventions GAD and Panic disorder Step 3 interventions GAD Step 3 interventions Panic disorder Back to stepped care table Individual non-facilitated self-help Facilitated self-help Psychoeducational groups Self-help groups CBT Applied relaxation Drug treatment Combined interventions Self-help groups CBT Antidepressants Self-help groups Stepped care: obsessive-compulsive disorder Step 2 interventions Individual CBT Group CBT (including ERP) Self-help groups Step 3 interventions CBT (including ERP) Antidepressants Combined interventions and case management Self-help groups Back to stepped care table Stepped care: post-traumatic stress disorder Step 2 interventions Trauma-focused CBT EMDR Step 3 interventions Trauma-focused CBT EMDR Drug treatment Back to stepped care table