Presentation on Depression and Anxiety
advertisement
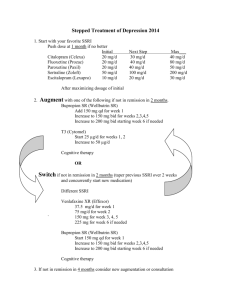
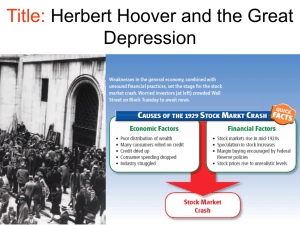
DEPRESSION and ANXIETY Dr. Khalid Aziz Consultant Psychiatrist Dennis Scott Unit, Edgware Community Hospital LEARNING OBJECTIVES Detection and diagnosis Advice on prevention Patient’s and carer’s expectations and concerns Care plan for treatment, recovery and crisis Consent and carer involvement Treatment guidelines Monitoring progress Cultural issues BEH trust’s services and clinical support Depression Pervasive low mood lasting two weeks or more Depressed mood, loss of interest, enjoyment and motivation Disturbed sleep, appetite, concentration Negative about self, world, and future, guilt Suicidal ideas, plans, intent, acts. Somatisation (more with age and in some cultures) Low energy, irritability, agitation. Anxiety Disorders Exaggerated concern about threat with avoidance Generalised vs episodic Panic disorder with/without agoraphobia Phobias (agora-, social, and specific) OCD PTSD May occur in the absence or presence of depression and other psychiatric disorders Physical symptoms of anxiety/panic. Prevalence Depression: 1 week prevalence 2007 was 2.3% Anxiety point prevalence 2 – 4 % 4-10% lifetime prevalence of Major depression 2.5-5% lifetime prevalence of Dysthymia 90% treated in Primary Care Large numbers un-diagnosed Cause of much absence from work Presumed underlying cause of suicides Ref. NICE guidance When to diagnose Duration – over 2 weeks Persistence – little variation each day Distressed by symptoms – varying degree Difficulty in functioning normally Presence of psychotic symptoms Ideas of self harm Differential Diagnosis Secondary to other physical or mental condition Adjustment disorder / Acute stress reaction Personality disorder Substance misuse Somatoform disorders Social triggers Grief If depression is present – treat it! What tools are helpful? PHQ-9 most common tool in Primary Care If score >= 10 - 88% chance of Major Depression Easy to administer Available QOF target How useful is it? Some useful questions How are you feeling in yourself? Can you rate your mood out of 10? (10 is “normal for you when you are OK”) Are you able to enjoy anything? Do you feel tired a lot? Ask about sleep and appetite How does the future seem to you? Suicidality Is life worth living? Do you wish you were no longer here? Do you get thoughts of harming or killing yourself? Have you made any plans about what you would do? Are you intending to act on these thoughts? Have you tried to harm or kill yourself? Is there anything particular that stops you? Any thoughts of harm to others? Suicide Best predictor is past risk behaviour Increased risk in men Increased risk if isolated Increased risk in chronic or painful illness Deliberate self harm not always a “cry for help”: 1 – 2% of dsh commit suicide in the subsequent year. When to treat Discuss with the patient Some want to wait longer than others – also depends on risk If in doubt, better to treat Type of treatment depends on severity and patient choice What treatments are available? NICE guidance recommends STEPPED CARE approach Severity graded Steps 1 – 4 Different options and recommendations for different steps: The stepped-care model Focus of the intervention STEP 4: Severe and complex1 depression; risk to life; severe selfneglect STEP 3: Persistent subthreshold depressive symptoms or mild to moderate depression with inadequate response to initial interventions; moderate and severe depression STEP 2: Persistent sub-threshold depressive symptoms; mild to moderate depression STEP 1: All known and suspected presentations of depression 1,2 see slide notes Nature of the intervention Medication, high-intensity psychological interventions, electroconvulsive therapy, crisis service, combined treatments, multiprofessional and inpatient care Medication, high-intensity psychological interventions, combined treatments, collaborative care2, and referral for further assessment and interventions Low-intensity psychosocial interventions, psychological interventions, medication and referral for further assessment and interventions Assessment, support, psycho-education, active monitoring and referral for further assessment and interventions Psychological interventions What is available? - CBT Counselling IAPT, MIND, Samaritans Local resources What should I do first? Explain your diagnosis Explain their symptoms Assess severity – use step guide + clinical impression If less severe, consider self-help approaches + monitoring Refer to IAPT or practice counsellor Start medication Treat any underlying cause(s) / physical health Primary Care follow up Arranging follow up appointment is containing (for both parties) Antidepressant response not usually seen before 2 weeks’ treatment Be aware of your reaction to the patient (overreaction, communicable anxiety, dismissing patient’s or carer’s concerns, only seeing the physical presentation) Medication NICE recommends SSRI as first line e.g. citalopram. Fluoxetine in adolescents Start with 10-20mg daily – depends on age etc. Need at least 6 week trial at treatment dose Try to avoid benzodiazepines or Z-drugs. If no benefit by 6 weeks increase dose and optimise to BNF limits before trying another class and monitor for 6 weeks at treatment dose. 6-12 months’ treatment after recovery 1st episode. Longer if recurrent Common side effects Nausea most common Dizziness Sometimes initial anxiety Sleep disturbance Sexual dysfunction (ejaculatory failure, anorgasmia) Withdrawal reaction – anx, insomnia, nausea Not dependence Not suicide (probably) Other good antidepressants Mirtazepine (NaSSA) good if poor sleep and poor appetite Few interactions Can cause weight gain Dose 15-45mg nocte Sedation not increased by increased dose (can be more sedating at 15mg) Other good antidepressants (2) Venlafaxine is allegedly SNRI – but only at higher doses Best used in secondary care Less safe in OD Lofepramine is the safest TCA start with 70mg daily, up to 210mg daily Important interactions Avoid SSRI’s with Aspirin or NSAID’s – GI bleeding risk Avoid SSRI’s with Warfarin or Heparin – antiplatelet effect Avoid SSRI’s with Triptans Mirtazapine safer in above situations When to refer Concerns about risk (suicide, dsh or self-neglect) Inadequate response to management in primary care Severe depression (psychomotor retardation, psychotic symptoms) “Gut feeling” Patient / carer preference Diagnostic question GP Advice Line – 020 8702 3997 Clinical Advice for GPs NEW GENERAL CLINICAL ADVICE LINE For a ten minute telephone clinical advice session with a Trust psychiatrist call the GP Clinical Advice Line 020 8702 3997 Mon-Fri (9am to 5pm) to book an appointment (same or next working day) and discuss generic issues relating to your practice on mental health. Where can I find out more? BEHMHT GP Intranet site – includes our more detailed treatment guidelines Barnet CCG website NICE Guidance RC Psych. website Any Questions?