Cumbria Partnership
An introduction to IAPT
Richard Thwaites - First Step Clinical Lead
May 2013
Plan
Introduce the IAPT Program
Explain roles and training
Why should IAPT services adapt what they deliver?
What are the challenges in IAPT services providing optimum experience of talking therapies for those with lower intellectual functioning?
Potential solutions…
What is the IAPT programme?
IAPT = Improving Access to Psychological Therapies (IAPT) programme
• Now has streams for Children and Families and also SMI, today we are talking about IAPT for adults in primary care
• a large-scale initiative that aims to greatly increase the availability of NICE recommended psychological treatment for depression and anxiety disorders within NHS
• Delivered within a stepped care framework
• Initially largely based around CBT (in line with NICE guidance) but expanding to include other evidence-based approaches (e.g. EMDR, IPT)
• Patients receive the treatments that research suggests that are most likely to work for them in line with best practice (e.g. appropriate training, supervision and ‘dose’)
Stepped care model for common mental health problems (e.g. depression )
STEP 4 : Severe and complex depression; risk to life; severe self-neglect
Medication, high-intensity psychological interventions, ECT, crisis service, combined treatments, multiprofessional & inpatient care
STEP 3: Persistent subthreshold depressive symptoms or mild to moderate depression with inadequate response to initial interventions; moderate & severe
STEP 2 : Persistent subthreshold depressive symptoms; mild to moderate depression
STEP 1
: All known and suspected presentations of depression
Medication, high-intensity psychological interventions, combined treatments, collaborative care and referral for further assessment and interventions
Low-intensity psychosocial interventions, psychological interventions, medication and referral for further assessment and interventions
Assessment, support, psychoeducation, active monitoring and referral for further assessment and interventions
What does IAPT provide?
• evidence-based psychological therapies (in line with NICE Guidelines)
• in a stepped care framework
• for individuals with a common mental health problem not requiring a multidisciplinary approach
Psychological Wellbeing
Practitioners
High Intensity Practitioners Primary Mental Health
Practitioners
Depression & Anxiety Disorders
(e.g. Panic Disorder, OCD, Health Anxiety, Generalised
Anxiety Disorder, Social Anxiety)
PTSD (HI Only)
Common mild to moderate mental health problems inc
Depression
Mild Eating Disorders
• Guided self-help
• Computerised CBT
• CBT
•EMDR (PTSD only)
• Brief CBT
• Counselling
Psychological Wellbeing Practitioners
- Delivering ‘low intensity’ interventions
• Usually shorter sessions (30mins, face-to-face or telephone)
• Support patients in the use of CBT-based guided self help
• Usually see the majority of patients
• High recovery rates
• Weekly Case Management Supervision
• Monthly Group Clinical Supervision
Psychological Wellbeing Practitioners
- Delivering ‘low intensity’ interventions
• Behavioural activation
• Cognitive restructuring
• Medication support
• Exposure therapy
• Problem solving
• Managing panic
• Sleep hygiene
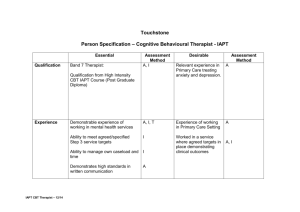
High Intensity Practitioners
- Delivering ‘high intensity’ CBT interventions
• Trained as CBT Therapists to work with depression and anxiety disorders (range of prof backgrounds)
• Usually ‘traditional’ length sessions (50-60 mins)
• Stepped to HI due to
• NICE Guidance e.g. PTSD
• Risk
• Failure to respond
• Deliver treatment in line with national IAPT protocols based on
RCTs
• One hour per week supervision from Accredited CBT Therapist
Measuring outcomes in IAPT
• The IAPT Minimum Data Set is nationally agreed
• Each session
• PHQ-9 (depression)
• GAD-7 (anxiety)
• W&SAS (work and social functioning)
• IAPT Employment questions
• IAPT Phobia Questions (anxiety disorders)
+ any Anxiety Disorder-Specific Measures
IAPT Recommended Outcome Measures
Disorder
Social Phobia
OCD
Outcome Measure
Social Phobia Inventory (SPIN)
Obsessive Compulsive Inventory (OCI)
PTSD Impact of Events Scale-Revised (IES-R)
Health Anxiety Health Anxiety Inventory (HAI)
Generalized Anxiety
Disorder
Penn State Worry Questionnaire
Panic/Agoraphobia Mobility Inventory (MI)
Why should IAPT services adapt what they provide for individuals with lower intellectual function?
• Numbers
• 1 in 5 and possibly up to 1 in 4 people with literacy and/or numeracy difficulties
• For First Step, potentially 2,600-3,250 individuals per year
• Moral argument
• Evidence-base
• Improve recovery rate
• And under Payment By Results increase income…
• Staff wellbeing/ satisfaction
What are the challenges for IAPT services in adapting services for individuals with lower intellectual function?
• Sheer volume of patients
• Admin systems that are effective at handling high volumes but flexibility is a challenge
• Massive clinical throughput
• High degree of performance management by commissioners
• Tight targets for assessment and treatment times
• Recovery rate targets
• High burden of measurement (e.g. MDS)
What are the challenges for IAPT services in adapting services for individuals with lower intellectual function?
• Emphasis on self-referral, staff often have limited information and do not know level of functioning
• Staff expert in evidence-based approaches but don’t necessarily have knowledge or experience of working with individuals with lower intellectual functioning
• Original training courses set up in a rush and many did not cover such issues
• Payment by Results/ Any Qualified Provider agenda
Potential answers to these challenges
• Communicate why equality of access is important
• Develop close links/pathways with your local LD colleagues
• Understand who is being referred to your IAPT service and who isn’t
• Being able to identify potential LD or lower intellectual functioning as early as possible
• Understanding and training staff
• Mapping outcomes of individuals with lower functioning
• Making key tweaks to what we do