Primary Mental Health Care and Wellbeing Service
advertisement
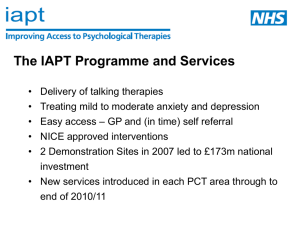
Primary Mental Health Care and Wellbeing Service Gordon King - Mental Health Commissioner Strategic Context • • • • • No Health Without Mental Health Care and Support Bill 2013 Healthier Northamptonshire Better Care Fund Think Local Act Personal (TLAP) 2 Mental Health Services in Scope • Emerging Primary Mental Health integrated SPoA • Primary Care Liaison function • Improving Access to Psychological Therapies including assessment, support, advice and brief therapy based interventions as part of PMH and WB • Mental Health Reablement/Prevention Services including short-term counselling, listening ear, short-term goal focused work, work experience and volunteering , low level supported accommodation. • Intermediate Support 3 Design Principles • To design and model a recovery based model of care which fully utilises and encompasses community assets. • To develop, implement and evaluate a clear and safe pathway for people transferring from secondary to primary care and vice versa. • To deliver quality outcomes for service users and carers. • To enable more people to be managed in a Primary Care setting. • To provide increased education for both people and their carers and health professionals around managing wellbeing 4 Emerging Model Primary MH GP/Practice team Treatment GP or Self Referral Urgent Care/ Crisis PCLW IAPT Secondary MH Social Care Step 0-1 Step 2 Step 3 Non-clinical signposting & support Bridging Interventions IAPT Specialist CBT/IAPT Care Navigators Peer Support Emotional Regulation Social Care Mindfulness Learn2B Groups / Individuals Specialist Peer Support (lived experience to model recovery) Social Care Recovery college Peer Support Community Resources Social Care Time Bank Psychiatrist / Nurse Prescriber for medication review Service Description • Single Point of Access for Primary MH based on locality model in community hubs • Mental Health promotion, information and signposting as part of wider hub/service • Assessment, problem identification and goal setting • Short-term support to address clear outcomes • Gatekeeping , referral and liaison with secondary mental health services • Enhanced Primary Care Psychological Therapies (based on NICE approach) 6 Expectations of Services • Integrated working across a wide range of agencies • Working in a flexible way to meet the needs of the individual ( Person centred) • Locality based and community focused working within the community hubs • Improved access and response for individuals accessing support at the closest point to people’s homes. • Reduce duplication of service delivery • Fully integrate with primary care and demonstrable link to secondary care 7 Outcomes for Individuals • A one stop local, accessible advice and support service that prevents needs escalating . • Increased improvement in mental wellbeing, resilience and recovery • Increased social participation and community integration • Increased choice in how to meet personalised outcomes • Increase in accessing training, volunteering and employment opportunities • Improvement in physical health. 8