Integrated Care
advertisement
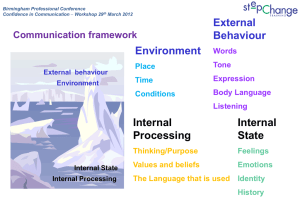
Developing Integrated Mental Health Services Professor Mervyn Morris CCMH BCU 31st MAY 2013 Where are we? UK West Midlands Region SCOTLAND LONDON WHERE PRINCE WILLIAM AND KATE LIVE Birmingham* mental health services Key Facts (2008-9) Population 1.2 m (including Solihull) Number of staff 3,924 Number of beds 722 Community Teams 79 Service users seen 48,459 *Birmingham and Solihull NHS Mental Health Foundation Trust Location of City’s 3 Premiership Football teams ASTON VILLA (Benteke) West Bromwich Albion (Lukaku) Birmingham City PRIMARY CARE (SUB) ACUTE Primary Care Liason ACUTE HOME TREATMENT Birmingham Model Functional Map CONTINUING NEED Rehab / Recovery CONTINUING NEED ASSERTIVE OUTREACH Residential based care: Hospital Beds, Day services, Crisis Houses, Belgium Functional Map of Adult Services PRIMARY CARE F1 (SUB) ACUTE F1/2a Primary Care Liason ACUTE F2a HOME TREATMENT Birmingham Model Functional Map CONTINUING NEED F3 Rehab / Recovery CONTINUING NEED F2b ASSERTIVE OUTREACH Residential based care: F4 Hospital Beds, Day services, Crisis Houses, Total mental health beds per 100 000 population (WHO Mental Health data From Atlas, 2011) 1:700 1:5000 What was Birmingham’s message? • It is possible to develop a full range of mental health services in the community that replaces the need for current levels of hospital provision. • Community services can develop different functions in the same way as hospitals and, like hospitals, can develop an integrated approach. • The community creates new opportunities because people and problems are ‘in vivo’. • The community creates different challenges because the system has less control than hospital. Three levels of an integrated system • Practitioners work in teams, not as individuals = Collaboration = Integrated Care • Teams work as part of an organisation of healthcare = Co-operation = Integrated Pathways • Health organisations work with other non-healthcare organisations = Co-ordination = Integrated Agencies Integrated Care – Integrated Pathways – integrated Agencies • Each team member, both as a person and by professional training, has a different view of the person, their problems and their situation. • Diverse thinking is important in making sense and finding solutions, but it is also important that the team works together (collaborate) to identify a common strategy and goal. Integrated Care – Integrated Pathways – integrated Agencies • It is important for the person, their family, and people they look to for help to know what service is available and how to access it. • Once connected to the service, everyone involved knows what help will be offered, and what continuing mental health service is available next. • Teams co-operate to agree who is responsible in what situation to prevent gaps in service, ensuring continuity of care. • An integrated pathway has similarities to a stepped care model. Integrated Care – Integrated Pathways – Integrated Agencies • Not all support for people with mental health problems is available from mental health services. Access to social care, social support, social housing, welfare payments, all require involvement of other agencies. • Co-ordination with other agencies ensures common agreement about longer term support and planning, ensures maximum use of resources, and prevents delay. Integrated Home Treatment • Specifically targeted to people who would otherwise go to hospital • 24 hours, 7 days a week, frequent, flexible visiting • Multi-professional team; doctors and nurses, social worker, occupational therapist, psychologist, community support workers • Rapid response, within 2 hours • Pathway from and back to community care • Gatekeeper to hospital • Crisis houses developed as alternative to hospital • In-reach to hospital for early discharge PRIMARY CARE COMMUNITY MENTAL HEALTH TEAM Primary Care Continuing Need: Liaison Rehab and Recovery HOME TREATMENT TEAM CONTINUING NEED ASSERTIVE OUTREACH TEAM Residential based care: Hospital Beds, Day services, Crisis Homes ‘Acute’ Care core pathway PRIMARY CARE COMMUNITY MENTAL HEALTH TEAM Primary Care Continuing Need: Liaison Rehab and Recovery HOME TREATMENT TEAM CONTINUING NEED ASSERTIVE OUTREACH TEAM Residential based care: Hospital Beds, Day services, Crisis Homes ‘Acute’ Care core pathway Data on 3 new teams, Birmingham 1995 Impact on Bed Usage Admissions Admission Home Treatment Home Treatment Reduction % 1 Year Pre 1 Year Post One 94 44 53% Two 96 50 48% Three 50 37 26% District Overall reduction in n. Admissions = 43% Data on 3 new teams, Birmingham 1995 Impact on Bed Usage Occupied Bed Days OBD* Home Treatment Home Treatment Reduction % 1 Year Pre 1 Year Post One 3,036 1,953 36% Two 3,667 1,662 55% Three 1,823 1,290 30% District Average reduction in n. bed days = 40% *OBD = OVERALL BED DAYS What have we learnt from supporting development in other countries? • There is existing community innovation and expertise that needs to be recognised and valued, but ultimately to be of value, becomes integrated. • Community and hospital psychiatry can have theoretical and ideological and differences, and this can impact on developing integration at all levels. • The way funding of services works is a big challenge; usually different services are paid for from different sources. It also means involving different government and local agencies. Developing Community Mental Health You can: • Develop a more differentiated community service, that reflects the traditional differentiation found in psychiatric hospitals. • Develop evidence to prove the care traditionally provided in hospitals can in many cases be provided in the community, more cost effectively, and with better patient outcomes. • Can make community care work for all types of ‘disorder’ and a higher level of ‘severity’. Some possible questions for Brussels.. • What is your overall vision for your services? • Can you describe your services using functional mapping? What stage are you at? • What does a functional map identify that you need to do in a short and long-term plan? Where are the gaps? • What is the priority at each level for developing services; teams, pathways, agencies? • What is practically possible.. next?