When Parents use
Methamphetamines: Strategies for
working with Children
Debra Eisert
OHSU and University of Oregon
Who I am
• Psychologist in CDRC clinic for 27 yrs
• Prof at U of O on disability projects.
• Member of group that organized
Methamphetamine workshop 2006
• Psychologist for BASE, a preschool
program to reunite parents and children
in foster care
Objectives
• Learn how prenatal methamphetamine
exposure impacts children
• Learn how methamphetamine use by
adult caretakers impacts children
• Strategies for addressing behavioral
challenges.
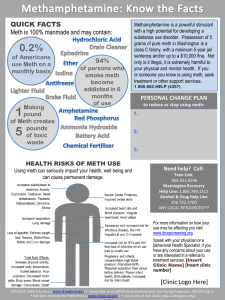
What is Meth
• Methamphetamine (meth, ice, crystal,
glass, speed, chalk, or tina) is a highly
addictive, man-made drug that
stimulates the pleasure section of the
brain.
• High lasts 6-24 hours
• Comes in Powder or Rock form
• Cooked from
ephedrine/pseudoephedrine plus
household chemicals
What does Meth Do?
• Meth causes the body to release
Dopamine, a neurotransmitter, which
results in pleasure or euphoria
• Depletes the dopamine stores
• Heavy users may not be able to
experience pleasure without the drug
• Produces a stronger, more lasting high
than cocaine
• People use Meth because they like
what it does to their brains
Images of meth use
Who Uses Meth?
• There are more than 1.4 million meth users
across the country.
• Was associated with blue collar white males,
but meth use occurs across all social classes
• High school and College students.
• Athletes
• More men than women
• More whites than minorities
Big Ideas
• It is difficult to separate effects of meth
exposure from other prenatal exposures,
because parents often use more than one
substance.
• Symptoms of prenatal exposure vary
depending on timing, amount and other
variables
• Some symptoms are not exclusive to drug
exposed children
Project FEAT, Shah, (no date)
Big Ideas (cont’d)
• Treatment is based on symptoms, not
exposure only
• Some symptoms may not be obvious until
after age two years.
• Risk of Exposure can be Balanced by stable
environment, and resilience factors
• Interventions depend on age, symptoms, and
individual characteristics
Different Sources of
Information
• Research is usually behind clinical
experience
• Experiences of medical professionals,
foster parents, child protective services,
therapists, teachers are valuable
• Longitudinal research is very important
• Can’t always separate impact of
substance use and environment
The Oregon Experience
• Oregon was one of the first states to have a
problem with Meth
• In 2004 and 2005, Oregon had 450 or more
meth lab incidents
• In 2004, Oregon adopted a rule where all
products containing pseudo-ephedrine must
be kept behind the pharmacy counter
• In 2005, the rule required ID and each sale
was logged.
Meth Use in the U.S.
The Oregon Experience
• In 2006, a new law required that the
cold medication be distributed only with
a prescription
• From 2004 to 2011, meth lab incidents
decreased from an average of 24 per
month to less than one per month.
• www.oregondec.org/OregonMethLabStats.pdf
Interpretation
• In 2010, Newsweek announced that
the meth epidemic in Oregon was
over, due to the restrictive law. But
• In 2012, the Huffington post
announced that the Cascade Policy
Institute had another perspective. It
seems that states surrounding Oregon
had a drop in admissions to treatment
centers and meth labs, without the law
in place in those states
• Methamphetamine is still available
because it is brought in from Mexico.
Still a problem
• Meth is still manufactured in California,
often by Mexican groups, and shipped
to Oregon.
• Some meth labs get around the law by
going out of state or having a small
army of buyers.
• As long as there are meth labs or meth
use, we should be concerned about
impact on children and adults
How does prenatal meth
exposure impacts children
• Children can receive different levels of
exposure, dosage and timing
– Prenatal
– Breastmilk
– Meth Labs and their chemicals
– Individual children may be impacted
differently
– Avoid stigmatizing terms like “meth baby”
Numbers of Substance Exposed
Newborns
• National prevalence data estimates that 1011% of all newborns are prenatally exposed
to alcohol or illicit drugs. This translates to
– An estimated 22,500 Oregon children ages 0-5
may have been substance exposed
– An estimated half of these children were exposed
to illicit drugs.
– In Oregon, in 2003, over 70% of foster care
placements were linked to Meth
– http://www.ncsacw.samhsa.gov/resources/substance-exposedinfants.aspx
Most Go Home from Hospital
• 80-95% of substance exposed infants
are undetected and go home.
– Obstetricians may not ask
– Hospitals may not ask, test or refer
– State Law may not require report or referral
– Tests only detect very recent use
– Robert Nickel, M.D. personal communication & NCSACW, 2006
Common Infant Symptoms
any substance exposure
• Hypertonicity– Infant massage, passive range of motion, ( after
training) Therapy if interferes with milestones
• Tremor
– Minimize stimulation, Swaddling, PT/OT?
• Irritability
– Avoid overstimulation, swaddling, pacifier, teach
self calming by sucking on fist, rocking horizontally
• Poor feeding regulation
– Nutrition consult, bottled water between feeding
(Shah, nd)
Common Infant Symptoms of
Meth Exposure
• In the first month, babies are often lethargic,
and not interested in feeding.
– Scheduled wakenings, foot massage to alert,
specialized nipples
• After the first month, babies often have
insomnia, dysregulated sleep, jitteriness,
irritability
– These babies need swaddling, reduced
stimulation, preparation for touch and holding,
• Foster parent college, substance exposed newborns
• http://health.utah.gov/meth/html/Healthconcerns/Children.html
How Does prenatal meth
exposure impact Children?
• IDEAL longitudinal study
– 1618 infants & moms, 84 with meth exposure
– Meth and non-meth exposed babies were also
exposed to alcohol, tobacco or marijuana use
– Meth group 3.5 X more likely to be small for
gestational age (SGA)
– Two times more likely to be premature
– Tobacco exposed group 2 X more likely to be
SGA compared to controls
–
Smith et al, 2006
IDEAL Cont’d
• Infants given Neurobehavioral scale
within first few days of life
• Babies had increased physiological
stress
• Heavy use associated with decreased
arousal, lethargy
• These moms were recruited at delivery,
which may affect memory of past use
Toddlers and Preschoolers
(any substance exposure)
• Speech Problems
– SLP evaluation plus intervention
– Read to child, language stimulation
– Signing after about one year of age
• Temper tantrums
– Normal toddler behavior or extreme?
– Use Redirection
– Communication strategies, behavior as
communication (reframe)
– Positive, non-punitive responses
–
Shah, Nd
Toddlers (Cont’d)
• Sensory Issues
– Desensitize to sensory issues (OT)
– Consider sensory treatment if the problem
interferes with development
– Avoid significant triggers
– Help child understand body cues and
emotions
– Predictable schedules
Toddlers (cont’d)
• Teaching children to tolerate low level stress
• Children benefit from low level exposures to
stress under supportive conditions
• If hungry, tired, learn that their cues will be
responded to.
• Power of Empathy
Case
• 2 1/2 year old boy seen in our clinic
• Physician for mom was unaware of her use
• Removed from home at 18 months due to
neglect, drug use, interpersonal violence.
Parents were jailed
• Second foster home
Case cont’d
• Prematurity, feeding issues, extreme
temper tantrums, speech/language
delays, distractibility, mood changes
• Cognitive skills in average range
• Speech/language delay
• Dysregulated sleep
• Anxious about relationships
Interventions for Child
• Consistent home environment, with
known caregivers
• Reduce overstimulation
• Divert attention when mildly upset
• Teach Self calming
• Consistent interventions across
caregivers
Interventions (cont’d)
• Feeding therapy
• Speech/language
therapy (EI)
• OT for sensory
problems
• Attachment therapy
• Good sleep hygiene,
monitor, consider
melatonin if needed
IDEAL
study ages 3 and 5
• 166 exposed and 164 non-exposed
tested at 3 and 5 years
• At 3 and 5 years - increased
emotionality and anxiety/depression
• At five years, more children had ADHD
• LaGasse, 2011, Pediatrics
IDEAL cont’d
• At age five years, Boys had more overall
externalizing problems, more inattention,
aggressive, ADHD, emotional reactivity,
withdrawal and total problems than girls
• Children of younger mothers had more
symptoms and poorer quality of home
environment was related to more symptoms.
Tobacco
• Tobacco was also related to increased
behavior problems, and withdrawal
symptoms (e.g., easily overwhelmed).
IDEAL Social Variables
• 43 children had two or more changes in
primary caregiver. 59% had at least one care
giver change by age 5
• 20% had low SES, 88 % had public health
insurance
• 7% exposed to domestic violence, and
reported child abuse (probably an underestimate due to caregiver report)
M Moms in IDEAL study
• More likely to be single,
• Live in household with < $10,000
income
• Tend to be younger,
• Have fewer, and later prenatal
visits
• Gain more weight
School-Aged children
(any substance exposure)
• ADHD
– Medication management
– Behavioral therapy
•
•
•
•
Reduce undesirable behaviors
Home school communication
Special Education Class
Parent/foster parent participation
• Shah, (no date)
Strategies for Addressing
School Aged Behavior
• Overall Intervention for Self-Regulation
• Adults should model their own stress
management (deep breaths in through nose,
out through mouth)
• Identify strategies for both structure and
flexibility
• Anticipate transitions and prepare
• Reward children for using self calming
• Avoid putting reactive children together
12 core principles for
Managing ADHD
• 1. Bridge or externalize time
• 2. Use immediate consequences for
positive or negative behavior
• 3. Frequent consequences 5 positives
to one negative
• 4. More intense, but not punitive
consequences
12 core principles (cont’d)
•
•
•
•
5. Vary the rewards to prevent boredom
6. ACT, don’t yack (no lectures)
7. Set up reward systems
8. Anticipate problems - prevent them
before they occur
• 9. Keep a disability perspective. ADHD
is a neurodevelopmental disorder
12 core principles
• 10. Maintain a set of priorities. Ignore
minor rule violations
• 11. Don’t personalize the child’s
problem. Maintain a sense of humor
• 12. Practice forgiveness, be a mother
not a martyr.
• (From Russell Barkley, no date)
School aged children
• Social emotional regulation
– Secondary diagnoses
– Trauma
– Team evaluation (educational or
medical)
– Classroom adjustments
– Permanency
– Counseling
How does methamphetamine use
by adult caretakers impact children
• Research on Children in Protective
services
• Research on What children can tell us
• Implications for foster families
Characteristics of some
parents due to meth use
•
•
•
•
•
•
•
Irritability,
paranoia,
sexual arousal,
days of highs and then sleep,
unpredictable and dangerous.
Criminal Activity,
domestic violence
Characteristics of Moms
(Any substance)
• New Zealand Study of Moms referred to
Alcohol and Drug Study Team (2001-2003)
• 33/34 moms used multiple drugs (tobacco,
alcohol, opiates)
• 14/34 did not keep medical appts
• 10/34 mental health problems, psychosis,
attempted suicide
• 7/34 had referrals to child welfare, custody
issues
• Wouldes, T., et al (2004). The New Zealand Medical Journal, vol
117.
Substance Use &
Trauma Exposure
• Examined children in child protective
services who had lived with someone
using meth, or with someone using
other drugs or children whose
caregivers did not use illicit substances
• Records of 1127 children
Results
• For most comparisons, Children exposed to
Meth were worse than the other groups on
–
–
–
–
–
–
Interpersonal violence
Child Endangerment
Physical abuse and
Chemical exposure
Out of home placement
More than 50% of children exposed to IPV
Additional sources of trauma
•
•
•
•
Weapons
Violence against siblings
Stranger violence
Removal from home and
decontamination if lived in lab
A word about Trauma
• Children who experience domestic
violence, parents who are irritable,
paranoid, sexually aroused, may
become traumatized
• Trauma is defined as experiences that
are outside the range of normal human
life.
Trauma
• When children are traumatized, they
may experience a prolonged alarm
reaction, which leads to altered neural
systems
• Children can experience increased
vigilance, alarm and fear
• These experiences can be impacted by
the proper supports
Trauma
• Trauma impacts how people think, behave and feel.
• Children may adopt behaviors that are functional in
the home environment but not in foster care.
• Children are may be hyper-aroused and tune out all
other information.
• Children may fight, scream, cry or they may appear
numb, and withdrawn
• Patterns may become ingrained
Treating Trauma
• Experienced Therapist
• Meta-analytic analysis of approaches indicated that
cognitive behavioral therapy is most effective
(Wethington, 2008)
• CBT is a combination of psychotherapy and
behavioral therapy that looks at maladaptive ways of
thinking, which can be modified with treatment.
Attachment
• Babies come into the world as
social magnets
• They are ready to understand
their social world
• But, babies who are born to
unavailable parents have more
difficulty regulating and
attaching
Attachment
• Babies use the state of mind of their
parent to understand their own state of
mind.
• Process over time
• Babies learn to make eye contact,
communicate needs, share affect,
engage in joint attention if parent is
available
Implications
• Babies developmentally aged 7-9
months can form selective attachments
• Must have substantial, sustained
contact
• May have qualitatively different
attachments
• Provides basis for other intimate
relationships
• Zeanah, et al 2012
Implications for foster parents
• Child Centered model
• Very young children in foster care
cannot maintain attachment to bio
parents based on short visits.
• Foster parents become the primary
attachment figures.
• Zeanah, et al, 2012
Implications (cont’d)
• Foster parents must care for the child as an
individual, psychologically as well as
physically
• Transitions must be carefully managed
• Stability must be valued
• Visits with bio parents and young children are
very stressful without foster parent proximity.
– Zeanah, et al (2011)
Neglect is Powerful
•
•
•
•
•
Health consequences
Psychological consequences
Relationship Difficulties
Behavioral consequences
Significant impact on attachments of
young children.
What Adults can tell us
• Interviewed 35 adult informants with a
variety of roles
• Informants described children’s
experiences of a rural drug culture with
antisocial beliefs and practices
• Rural counties in the Midwest
• Meth use as a subculture
• Haight et al (2005), In these bleak days . . .
“In these Bleak Days
• Children develop antisocial beliefs and
practices through
• Exposure to danger, lying and stealing
• Drug use and violence
• Children as lookouts
• Children told not to talk about the drugs
Individual differences
• Differences may be due to:
– Temperament, intelligence, resilience
– Extended Family
– Community (e.g., school practices)
Children’s voices
• Interviewed 18 children ages 7-14 in foster care due
to meth use by parents
• Children are frightened and sad about their parents
use and about involvement of law enforcement.
• May describe parents as mean, hyper, fighting,
psychotic.
• May follow parent directions to not talk, to deny meth
use by parents. They may believe parents were “set
up.”
• Haight et al, (2007)
Children’s Reports(cont’d)
• Observed Violence between adults,
• Physical abused by parents or adults
• Involvement in illegal activities, sex,
drugs
• Fearful of “being taken”, resist supports
from foster family (Haight et al 2007)
Children’s perspectives on
foster families
• Children may resist making connections to foster
families
• If parents in prison, children face long stays in foster
care
• Have lived semi-independently, had adult roles
• Have cared for their younger sibs
• May Resist rules and routines and monitoring
• Resist foster families attempts to care for them.
– Haight et al, 2007
Implications for Foster Families
• Expect divided loyalties and don’t make
older children choose
• Supportive, empathic talk for child
• Expect and prepare for upset.
• Clear rules with flexibility
• Provide normalization
• Individual/Family therapy if available.
A Paradigm Shift
• It is time to view child abuse and parent
chemical dependency as a multigenerational legacy family that can only
be healed by defining “the client” as “the
family”
– Susie Dey, Director of Child and Family
Services at Willamette Family Treatment,
40 years experience in child
welfare.(Project FEAT)
Community Based Strategies
• Project FEAT at the U of Oregon
• Jane Squires and Robert Nickel,
Directors.
• Improve outcomes for substance
exposed newborns
• Target Systems Change in Lane County
– http://eip.uoregon.edu/projects.feat
Project FEAT identified five points
for potential intervention
•
•
•
•
•
Pre-pregnancy awareness
Prenatal Awareness
Identification of Child and parent at birth
Infant Safety and Parent treatment
Link Systems to support child and
Parent throughout development
Lane County Activities
• Lane County Interagency collaborative
workgroup
• Family Advocate
• State level collaboration
• Ongoing evaluation
Established workgroups
•
•
•
•
Prenatal screening
Hospital Policy
Substance exposed newborn team
Postnatal supports
• Project FEAT
Substance Exposed Newborn
• Multidisciplinary team convened at the
hospital to give input into placement
decisions
• Family Advocate to provide intensive
intervention services to pregnant
women and new moms with substance
use issues
• http://aia.berkeley.edu/training/SEN2010/sen_agen
da.php
Final Recommendations
• Enhance supports in school and local
community
• Timely involvement of Child welfare
• Timely access to quality mental health
services that address mental health
assessment, trauma, normalization
• Understand the subculture of meth
users and developmentally appropriate
practice.
Interdependence is critical
• Teachers may be first to note neglect,
or others signs of use
• Schools provide clothing, food &
toiletries. Schools as normalizing, safe
places.
• Communication between child welfare,
police, county law enforcement.
• (Haight et al 2005)
Questions?