Consultation Models - Swindon GP Education
advertisement
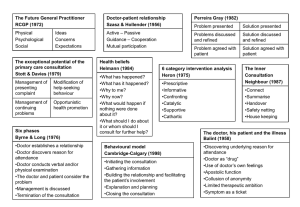
Consultation Models Introduction • Models enable the Dr to think where in the consultation the problems are, • There are lots of models. • Task orientated, Skills based, • • Some are based on the doctor patient relationship, or the patients perspective of illness. What models do you know? Consultation models • 1957 M Balint - The Doctor, His Patient and The Illness • 1964 E Berne - Games People Play • 1975 Becker & Maiman - Sociobehavioural Determinants of • • • • • • • • • Compliance ... 1975 J Heron - Six Category Intervention Analysis 1976 Byrne & Long - Doctors Talking to Patients 1977 RCGP definition - Physical, psychological & social ... 1979 Stott & Davis - The Exceptional Potential in Each Primary Care Consultation 1981 C Helman - Disease vs Illness in Gen Practice 1984 Pendleton et al - The Consultation 1987 R Neighbour - The Inner Consultation 1987 R C Fraser - Clinical Method: A Gen Pract Approach 1996 Kurtz & Silverman The Calgary-Cambridge Observation Guide to The Consultation Traditional medical model The classic medical diagnostic process involves the following steps: • observation - history and examination • hypothesis -provisional diagnosis • hypothesis testing - investigations • deduction - definitive diagnosis. Balint -1957 • Hungarian doctor and psychoanalyst • Founded with his wife Enid in the 1950 • This experince led to his book “The Doctor, his Patient and the Illness“ • Balint groups Balints consultation approach • Psycological problems are often manifested physically and physical disease has psychological consequences • Passing responsibility of dealing with a problem on to someone else was defined by Balint as“collusion of anonymity“ Balints consultation approach • Doctors have a therapeutic role in the consultation : drug doctor • Doctors feelings have a function in the consultation • Balint describes the „Flash technique“: the doctor becomes aware of his feelings and interprets this back to the patient Transactional Analysis Eric Berne 1964 T-A model This model discusses the 3 “ego-states” • Parent - critical/caring. • Adult – logical. • Child – dependent. Believes human psyche is influenced by mother and infant intimacy and that infant style intimacy can develop in certain relationships including dr-pt. T-A model Useful to recognise when a dr-pt relationship develops into a parent-child dynamic. Consultations may develop into games where the pts interests are not served. Need to try to recognise the new dynamic and try to have both dr and pt take on the adult role. DVD case 5 Helman • 1) What has happened? This includes organising the symptoms and signs • • • • • • into a recognisable pattern, and giving it a name or identity. 2) Why has it happened? This explains the aetiology or cause of the condition. 3) Why has it happened to me? This tries to relate the illness to aspects of the patient, such as behaviour, diet, body-build, personality or heredity. 4) Why now? This concern the timing of the illness and its mode of onset (sudden or slow) 5) What would happen to me if nothing were done about it? This considers its likely course, outcome, prognosis and dangers. 6) What are its likely effects on other people (family, friends, employers, workmates) if nothing were done about it? This includes loss of income or of employment, or a strain on family relationships. 7)What should I do about it or to whom should I turn for further help? Strategies for treating the condition, including self-medication, consultation with friends or family, or going to see a doctor. Roger Neighbour – The Hand • 5 checkpoints – Connecting – Summarising – Handing-over – Safety-netting – Housekeeping • Inner consultation – “2 heads” – the Organiser and the Responder Role play in 2 groups, one group looking at Helmans model, the other looking at Neighbours model • Helmans • • • • • • • What has happened? Why has it happened? Why has it happened to me? Why now? What would happen to me if nothing were done? What are its likely effects on other people (family, friends) if nothing were done 7)What should I do about it or to whom should I turn for further help? • Neighbour – – – – – Connecting Summarising Handing-over Safety-netting Housekeeping –Pendleton, Schofield, Tate and Havelock (1984) – – – – – – – – – – – – – – – – – (1) (2) (3) (4) (5) (6) (7) To define the reason for the patient’s attendance, including: i) the nature and history of the problems ii) their aetiology iii) the patient’s ideas, concerns and expectations iv) the effects of the problems To consider other problems: i) continuing problems ii) at-risk factors With the patient, to choose an appropriate action for each problem To achieve a shared understanding of the problems with the patient To involve the patient in the management and encourage him to accept appropriate responsibility To use time and resources appropriately: i) in the consultation ii) in the long term To establish or maintain a relationship with the patient which helps to achieve the other tasks. consulting styles In the doctor-centred consulting style, the doctor: • dominates the consultation • asks direct, closed questions • rejects the patient's ideas • evades the patient's questions In the patient-centred consulting style, the doctor: • asks open questions • actively listens • challenges and reflects the patients' words and behaviour to allow them to express themselves in their own way The Calgary-Cambridge approach to communication skills teaching (1996) • Suzanne Kurtz & Jonathan Silverman • Doctors and patients tend to carry out the four tasks of initiating the session, gathering information, giving information and closing the session roughly in sequence while relationshipbuilding is performed continuously during the other tasks. Initiating the Session Gathering information Providing Structure Building the relationship Physical Examination Explanation and planning Closing the Session Initiating the Session • preparation • establishing initial rapport • identifying the reason(s) for the consultation Gathering information Providing • exploration of the patient’s problems to discover the: Structure biomedical perspective • making organisation overt Building the relationship the patient’s perspective background information - context • using appropriate non-verbal behaviour • developing rapport • involving the patient Physical examination • attending to flow Explanation and planning • providing the correct amount and type of information • aiding accurate recall and understanding • achieving a shared understanding: incorporating the patient’s illness framework • planning: shared decision making Closing the Session • ensuring appropriate point of closure • forward planning