The Family
advertisement
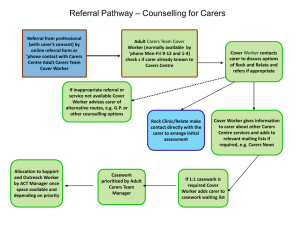
The Family: A Help or Hindrance to the Rehabilitation Process? Dr Anita Rose Consultant Neuropsychologist & Director of Clinical Service Outline • Family Involvement – What is it – Need for it • Empirical evidence – Reasons to involve – Barriers • How Titleworth have responded • Family involvement in Acquired Brain Injury (ABI) rehabilitation is a developing area • Services more aware of the need to involve family and working towards ways of developing involvement • Anecdotal reports and opinion papers suggest ways that family involvement might improve the rehabilitation outcomes for patients (Tarvin, 1995) • Recent government policy documents have called for more focus recognising the expertise of the carer and greater involvement of the family in the rehabilitation process after ABI – Caring about Carers (DOH, 1999) - “helping carers is one of the best ways of helping people they are caring for” (p6) – National Carers Strategy (DOH, 2008) states that by 2018: “carers will be respected as expert care partners and will have access to the integrated and personalised services they need to support them in their caring role” (p9) What could family involvement mean in ABI? • Determine the success of the transition phase from hospital to home • Facilitate the carryover of rehabilitation strategies to compensate for cognitive difficulties (Fleming, Shum, Strong & Lightbody, 2005; Turner et al., 2007). • Potentially reduce the length of time required in hospital • Reduce costs of rehabilitation (Kalra et al., 2004) • Resolve issues related to family adjustment (for example when a family member may have unrealistic expectations regarding their relatives’ recovery) What does family involvement mean? • Very varied when look at empirical literature and service documentation, includes: – involvement in goal planning – acting as a co-therapist – “otherwise involved” – Involved in therapeutic activities – involvement in discharge planning • Few guidelines available on how clinicians should involve families in goal planning (Levack et al 2009) • A recent review of goal planning in the rehabilitation centres in the United Kingdom, found that carers were not always routinely involved despite national recommendations (Monaghan, Channell, McDowall & Sharma 2005) • Family involvement does not always happen in practice and services may only pay lipservice to this despite the recommendations in government policies (Levack et al., 2009; Brereton & Nolan, 2002; Monaghan et al., 2005) • Important to determine what factors may facilitate or prevent families’ engagement or involvement in order for rehabilitation services to address these and improve the consistency across services. Inconsistencies between staff and family perceptions • Shaw et al. (1997) found that the staff and family members differed in their opinions regarding family involvement. – Agreement that information should be shared, but differed in opinions • family involvement in treatment planning • involvement in therapies • regarding education – in particular families felt that the education should be more specific to their relative’s condition rather than more general information Recognition of /lack of recognition of the carers’ expertise and knowledge • Brereton and Nolan (2002) identified the relationship and communication between staff and families as a potential barrier or facilitator to family involvement – Families expressed a wish to be more involved in their relatives’ care – reported that they actively made attempts to form partnerships with health professionals in order to gain confidence and acquire skills to be able to carry out care activities with their relatives – these attempts were not always acknowledged or were rebuffed some families reported that they felt they were intruding on professional territory when they tried to get involved – Families also expressed a need for their knowledge to be recognised and valued Family involvement in Rehab Therapies • One study investigated physiotherapists perceptions of family involvement in the rehabilitation process. (Ryan et al. 1996) • Four main factors that impeded: – Family – Therapist – Healthcare Organisation – Patient • Other factors included: – Families availability/flexibility – Cognitive skills – Financial status – Emotional health – Relationship with patient – Unrealistic expectations (particularly of family) – Experience and confidence of therapist with involving family • Galvin, Cusack and Stokes (2008) found similar results Family involvement in Goal Planning • Involving family members in decision-making processes such as goal planning can make the family more willing to engage in the rehabilitation process (Levack, Dean, Siegert & McPherson 2009) • Family as an integral part of the goal planning process provides an opportunity to families about rehabilitation principles. • Early discussion of goals could help to prevent conflict from arising at the stage of discharge and to aid the development of realistic expectations of recovery and emotional adjustment • Has to be acknowledged there are barriers to family involvement: – Family members had their own agendas – Expectations were unrealistic – Clinicians feeling have to limit family involvement, or avoid engaging with the family at all to protect the patient • Overall research indicates that clinicians are more oriented to addressing the needs of patients rather than the family Family involvement in discharge planning • Relatives and health professionals may have different expectations regarding goal setting (Almborg, Ulander, Thulin and Berg 2009) • Therefore there is a need to develop more effective discharge planning procedures to include provision of information so that they can be more involved in the rehabilitation process • Services may lack effective practice for involving families Conclusion of Empirical Review • Some evidence, albeit limited, regarding the effectiveness of family involvement in improving the outcomes of their relatives • There is a need for more high quality research to prove its effectiveness and to ensure that family involvement is seen as important by all parties and incorporated into routine care • A need for services to address staff and organisational barriers • A need for training and education to change attitudes and practice in working with families and accountability for ensuring family involvement in routine aspects of rehabilitation • Barriers to carer involvement could also focus on addressing the needs of families, who may feel that they lack the skills to make a meaningful contribution, which could therefore limit their engagement and involvement in their relative’s rehabilitation. Clinical/Service Implications • Process of rehabilitation for neurological patients can place demands on family • Family adaption in chronic illness or injury has been likened to “navigating uncharted territory” (Steele, 2005) • Carer burden and strain “high level” • Divorce/ Separation very high (Webster et al., 1999) – Although research in 2007 indicates this might not be higher than generic population (Kreutzer et al.) • Adjustment to traumatic and acquired brain injury tends to be more demanding for spouses because the person who returns home from hospital can pose specific difficulties (Serio et al, 1995) • Involving families in Rehabilitation of their loved ones can help aid adjustment and outcome • Providing intervention/support for families very important • Responsibility to educate providers and commissioners in need to “provide” for family members as an vital part of rehab process The Titleworth Experience • It was acknowledged there is a need for the service to take more active steps to: – Actively involve all family members, significant others etc in care and daily life of each resident • Directly • Indirectly – Actively manage family expectations to avoid the extremes of optimism and pessimism • Education – Formal – Informal – Actively manage family adjustment to ABI • Therapeutically • Practically • Educationally – Actively engage commissioners and providers in understanding the need for support of families • Discussions at referral/admission time • Reviews • Changes of residents’ needs How do we do it? • Family meetings – Friends of Mulberry • Open door policy – – – – • • • • Access to manager, neuropsychologist, staff Meal times Family parties Activities Reviews, goal planning, discharge planning Resource files Education Research Dealing with Inconsistencies • Empirical evidence highlights this as a major issue • Experience was miscommunication/lack of communication was evident at times • Action: – Speak to families at point of referral (regardless of whether referral goes active) – Invite families for a visit (regardless of whether referral goes active) – Prior to admission involve families in plan of treatment • gain information about enjoyable activities etc – Involve in therapies if resident and family happy to be • Teach strategies e.g. physio – Involve in appointments • If not possible written record provided – Open door • • • • • • Families can visit at any time Encourage open discussion with all staff Comments Book Regular surveys Family meetings Involvement in menus, patio planning etc etc. – Invited to ALL goal planning and review meetings – Any concerns immediate phone calls • Families are reporting feeling significantly more involved and feel they have open communication channels and that the previously miscommunication issues no longer a problem. Recognition of Carer expertise • “By 2018 carers will be respected as expert care partners and will have access to the integrated and personalised services they need to support them in their caring role” National Carers Strategy (DOH, 2008) • Acknowledged by families often their opinion not considered • Families of residents felt this not a particular issue however changes made • Action: – Speak to families at point of referral (regardless of whether referral goes active) – Invite families for a visit (regardless of whether referral goes active) – Prior to admission involve families in plan of treatment • gain information about enjoyable activities etc – Any change in resident e.g. behaviour, compliance etc. speak to family if unable to communicate with resident – Best Interests meetings – Listen to concerns – Care Plan Involvement in Rehab Strategies • It is recognised there are a number of barriers – – – – Availability Desire Organisational Therapist • Action – Willingness to change therapy time to accommodate family – Psychotherapy for family – Family therapy – Providing support to families when go out • Very detailed written leave guidance regardless of length of leave • Sending staff Involvement in Goal Planning and Discharge Planning • Recognised that to enable engagement and address unrealistic expectations important to involve family • Action – Invite to all meetings – Willingness to accommodate at a time suitable (although barrier can be external agencies not so willing/able) – Accommodation can be sourced if coming from a distance – Minutes and reports sent out within 48hrs – Requests for information prior to meeting if not able to attend – Indirect education provided about ABI via GP meetings Education Programme • Research and own investigation highlighted education need around own family member as well as/as opposed to general – Open door attitude – All resident meeting – Have resource files and documentation always available to families to help with understanding of their loved one’s difficulties – Modular training so all staff confident in providing – Family module to be run – Indirect modes – general conversations, therapy times, family meetings – Current research projects How we see our role To help our residents and families navigate uncharted territory