Reducing Behavioral Restraint & Seclusion & SB 130
The Basics of Behavioral
Restraint and Seclusion
Leslie Morrison
Director, Investigations Unit
Disability Rights California
(510) 267-1200
Leslie.Morrison@DisabilityRightsCA.org
February 2013
1
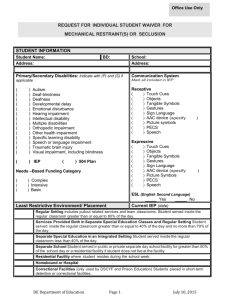
Defining Terms
Seclusion
Restraint
Restricting freedom of movement, physical activity or normal access to one’s body
Medical
Postural/Supportive
Behavioral
Physical force; manual holds
Mechanical device, material or equipment
Chemical [drugs]
Not:
2
Briefing holding to calm or comfort
Brief assistance to redirect or prompt
Devices used from transportation or security
Involuntary confinement alone in a room or an area from which the resident is physically prevented from leaving
Doesn’t matter if door is locked or even closed
Not:
Voluntary time out
Restriction to area consistent with unit rules or an individual’s treatment plan
What is “ chemical restraint ”?
Medication used as a restriction to manage an individual’s behavior, generally unplanned and in emergency/ crisis.
Not medication routinely prescribed to treat individual’s psychiatric condition to improve functioning.
Not necessarily all PRNs but often PRNs are used.
Often used in combination with other forms of restraint or seclusion.
3
What we
know
about restraint and seclusion…
4
Have no therapeutic value or basis in clinical knowledge.
Does not positively change behavior
May increase negative behavior and decrease positive behavior.
Is traumatic and potentially physically harmful to staff and the individual.
Does not keep people safe.
May cause death even when done “safely” and correctly.
Leaves lasting psychological scars.
Decision is almost always arbitrary, idiosyncratic, and generally avoidable.
Facility culture (staff role perceptions, training, program philosophy, facility leadership) has greater influence on the use of restraint & seclusion than clinical factors.
Restraint and seclusion is often staff’s first, automatic response to difficult behavior.
Generally stems from a power struggle .
Mostly used for loud, disruptive, non-complaint [but not violent] behavior.
Lack of training in managing behavioral crisis contributing factor 90% of JCAHO restraint deaths.
Myths/Assumptions
vs.
Reality
Keeps people (staff
& consumer) safe
Known to cause injury, death and last psychological trauma;
Higher worker injury rate than in lumber, construction and mining
Only used when absolutely necessary and for safety reasons
Most often used for non-compliance, inappropriate behavior or power struggle
(1) study 73% (560 consumers) not dangerous but
“inappropriate” at time restrained/secluded
Staff can recognize potentially violent situations
Nurses agree on use 22% of time; mental health professionals can only predict violence potential 53% of time; least clinically experienced were most restrictive
Staff know how to deescalate
De-escalation used < 25% of time;
Most frequent antecedent was staff-initiated encounter = staff escalate;
Lack of training in managing behavioral crisis contributing factor 90% of JCAHO restraint deaths;
1/3 of staff surveyed didn’t get mandatory crisis training
Used without bias and only in response to objective behavior
Cultural and social bias, staff role perception, administrator attitudes
Therapeutic and based on clinical knowledge
No controlled studies, no measure of efficacy or therapeutic value; shown to increase negative behavior
Restraint/seclusion used for safety not punishment
(6) studies = 58-75% perceived as punishment
6
Whose Pre-disposed?
No “typical” patient profile
No consistent demographics
No consistent clinical characteristics
Although individuals w/trauma or abuse history at greater risk…
√ Staff profile
Mostly used for loud, disruptive, non-complaint behavior
Generally stems for power struggle
Based on cultural bias & staff perception
Belief that it is safe/harmless & reduces risk of injuries
√ Facility culture
Automatic response to difficult behavior
Insufficient alternatives
Insufficient staff training in de-escalation
Little to no focus on reduction; not seen as a critical event/ treatment failure
7
Dangers
Psychological
Physiological
Death
Asphyxiation
Strangulation
Aspiration
Cardiac and/or respiratory arrest
Fractures, dislocation/sprains
Lacerations, abrasions
Injury to joints and muscles,
Dislocation of shoulder and other joints,
Hyperextension or hyperflexion of the arms,
Overheating, dehydration, exhaustion,
Exacerbation of existing respiratory problems,
Decreased respiratory efficiency,
Decrease in circulation to extremities,
Deep vein thrombosis,
Pulmonary embolism,
Cardiac and/or respiratory arrest.
Last psychological trauma
Loss of dignity
Triggering flashbacks
Recurrent nightmares, intrusive thoughts, avoidance behaviors,
Enhanced startle response,
Feelings of guilt, humiliation, embarrassment, hopelessness, powerlessness, fear, and panic
Compromised ability to trust and engage with others,
Environmental
Creates a violent and coercive environment that undermines forming trusting relationships
Risks with Medication
Sedation contributing to respiratory depression & arrest
8
Conditions on Use
Only used:
◦
◦
◦
◦
◦ in emergencies, to prevent imminent risk of physical harm when other less restrictive alternatives have failed, for the least amount of time necessary, and in least restrictive way.
Never for coercion, discipline, convenience or retaliation by staff
Only by staff with specific, current training and demonstrated competence in application
Only upon MD order OR , in emergency, at discretion of RN
◦
◦
Never as a standing order
Limits on order duration
◦
◦
Face to face assessment by MD or specially trained RN/PA within one hour [at hospital]; other timeframes apply for other settings
Requires certain level of monitoring or observation
Where & What are the Standards ?
Federal law
Hospitals
Residential Facilities for
Adolescents
State Law and Regulations
By facility type
Joint Commission
Not all facilities
By facility type
What standards?
Duration of orders
Type of observation frequency of monitoring
MD consultation & oversight
Documentation requirements
Staff training elements
Reporting requirements, data collection
Quality Improvement criteria
10
Additional State Requirements
Health & Safety Code §1180
Prohibits risky practices:
Obstruct airway or impair breathing
Pressure on back or body weight against back or torso;
Anything covering mouth;
Restraint w/known medical or physical risk if believe it would endanger life or exacerbate medical condition;
Prone with hands restrained behind back;
Containment as extended procedure
If prone, must observe for distress
Prone mechanical restraint with those at risk for positional asphyxiation, unless written authorization by MD .
Intake assessment with consumer input
Advanced directive on deescalation or use of R vs. S
Early warning signs/ triggers/precipitants,
Techniques that help person maintain/regain control,
Pre-existing medical conditions, trauma history.
Post-Incident Debriefing
ID & understand precipitant(s);
Alternatives/other methods of responding;
Revise plan to address root cause;
Was it necessary & done right?
11
Data
How does a facility prevent R/S?
CHANGE THE CULTURE:
From Control → to Empowerment
Involvement by top leadership
Create a vision and culture that prevents the risk of conflict and violence and respects personal liberties
Maintain sufficient staffing & programming
Keep reduction in use & duration as constant priority and focus
Integrating the principles of recovery and trauma informed care
Implement restraint/seclusion prevention tools & alternatives
Trauma assessments
Crisis plans
12
Comfort rooms
Sensory modulation tools
Workforce development
Build relationships
Avoid power struggles
Built into staff competencies and performance evaluations
On-going training (not only point in time)
Rigorous debriefing of every incident with involvement of senior administration
Use data to inform practices
Public reporting & posting
Rigorous analysis
Actively Recruit & Involve Consumers and Families
Peer advocates in debriefing
Facility committees & positions
13
Principles of Trauma-Informed Care
Program and services based on:
Understanding vulnerabilities and triggers of trauma survivors that can be triggered in traditional service delivery systems
Designed to be supportive and avoid re-traumatization
Respect individuals.
Keep them informed, connected and hopeful about their recov ery
Work collaboratively in a way that empowers the individual.
Learning together vs. Helping (one individual has agenda for the other)
Relationship vs. the Individual
Responding out of Hope (caring, patient, & supportive) vs.
Reacting out of Fear (rule driven, reactive, restrictive)
Public Health Model
focus on prevention NOT how to do more safely or better
Universal Precautions
Administrative & clinical treatment environment that minimizes potential for conflict by anticipating risk factors
Trauma informed care
Recovery Model
Stigma awareness
Early assessment of risk factors
Organizational values
Secondary Intervention
Immediate & effective early intervention strategies to minimize conflict and aggression when they occur o Individual assessment of risk o Individual crisis plans to teach emotional self-management o De-escalation skills
Tertiary
Intervention
After incident, rigorous problem solving, mitigate effects, take corrective action
Post S/R interventions to mitigate effects
Debriefing
Corrective Action o Staff training on attitude & self-awareness during conflict o Sensory modulation tools o Comfort rooms
15