F4b - Collaborative Family Healthcare Association
advertisement

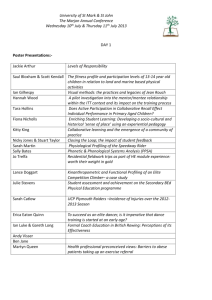
Session #F4b Saturday, October 18, 2014 Cost Assessment of Collaborative Healthcare Shandra Brown Levey, PhD, Clinical Psychologist Emma Gilchrist, MPH, Project Manager Warren Pettine, Medical Student University of Colorado Denver Department of Family Medicine Collaborative Family Healthcare Association 16th Annual Conference October 16-18, 2014 Washington, DC U.S.A. Faculty Disclosure • We have not had any relevant financial relationships during the past 12 months. Learning Objectives At the conclusion of this session, the participant will be able to: • Describe a novel approach to calculating the cost of integration. • Discuss the benefits of a multidisciplinary team in developing integrated care initiatives. • Identify the policy implications of assessing cost for integrated care. Bibliography / Reference 1. Chapkoa MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009; 18: 1188–1201 2. James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Affairs. 2011;30(6):1185-1191. 3. Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harvard Business Review. 4. Katon W, Russo J, Lin EH, et al. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Archives of general psychiatry. 2012;69(5):506-514. 5. Manderscheid RW, Alexandre P, Everett A, Leaf P, Zablotsky B, Eaton W. American mental health services: perspective through care patterns for 100 adults, with aggregate facility, service, and cost estimates. Public mental health. 2012:381. 6. Porter ME. What is value in health care? New England Journal of Medicine. 2010;363(26):2477-2481. 7. Ritzwoller DP, Sukhanova A, Gaglio B, Glasgow RE. Costing behavioral interventions: a practical guide to enhance translation. Ann Behav Med. Apr 2009;37(2):218-227. Learning Assessment • A learning assessment is required for CE credit. • A question and answer period will be conducted at the end of this presentation. CoACH Origins • Prescription for Health/ACT/SHAPE • Work with practices to determine the cost of integrating to determine a global payment • CoACH automates this process and provide a tool for interested practices to determine financial factors and workflow associated with integration activities Developed by multidisciplinary team – – – – – – Psychology Public Health Economics Actuarial Science Biostatistics Integrated Primary Care Practices • Input from primary care providers, behavioral health providers, practice managers, medical assistants, front desk staff, CFOs, administrators CoACH: Cost Assessment of Collaborative Healthcare • On-line tool to determine the estimated incremental expenditure of integrating behavioral health and primary care. • Practices are asked to work with others in their organization for improved accuracy of estimates. • Practices receive: • an estimated incremental expenditure to complete the work proposed • the building blocks for an accurate and adjustable workflow • average reimbursed amounts across payer types based on the Colorado APCD data by month and year Some information CoACH requires • • • • • Payer mix percentages by practice Estimations for FTE of involved personnel Average monthly mid-point salaries and benefits Number of patients in the practice Types of collaborative or integrated care activities the practice currently does or plans to do • Estimated time per week providers and staff participate in integrated care activities Tips for Completing CoACH • CoACH can be paused and returned to using a link sent to the email address practices provide. • Working with a team to complete CoACH can help improve accuracy input regarding integration activities, personnel responsible for activities, and activity time approximations. Policy Implications • All participants in the health care system need objective, evidence-based information to make critical decisions about how to allocate health care resources. o o o o o o Employers Insurers Patients Providers State Policymakers Federal Policymakers Session Evaluation Please complete and return the evaluation form to the classroom monitor before leaving this session. Thank you!