Chapter 5
*Lecture Outline
*See separate FlexArt PowerPoint slides for all
figures and tables pre-inserted into PowerPoint
without notes.
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chapter 5 Outline
•
•
•
•
•
•
•
Structure and Function of the Integument
Epidermis
Dermis
Hypodermis
Accessory Organs
Repair and Regeneration
Aging and Development
Intro to the Integument
•
Integument = skin
–
–
largest organ (7% to 8% of body weight)
two layers
•
•
epidermis: superficial layer of stratified
squamous epithelium
dermis: deeper layer of areolar and dense
irregular connective tissues
– hypodermis (not part of the skin) lies
under dermis, mostly adipose
connective tissue
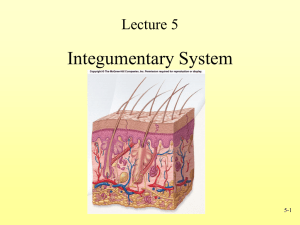
The Integument
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hair shaft
Sweat pore
Epidermis
Epidermal ridge
Dermal papilla
Papillary
layer
Arrector pili muscle
Sebaceous (oil) gland
Sweat gland duct
Dermis
Reticular
layer
Merocrine sweat gland
Sensory nerve fiber
Apocrine sweat gland
Vein
Artery
Subcutaneous
layer
Adipose connective tissue
Figure 5.1
Hair follicle Sensory
Areolar
receptors connective tissue
Integument Functions
•
•
•
•
•
•
•
Protection
Prevention of H2O loss
Temperature regulation
Metabolic regulation
Immune defense
Sensory reception
Excretion/Secretion
The Epidermis
• Most superficial layer
• Avascular
• Keratinized stratified squamous epithelium
– keratin is a water-insoluble protein
– 4 to 5 layers (strata) of distinct cell types
Epidermal Strata
•
From deep to superficial (as they grow):
–
–
–
–
–
stratum basale
stratum spinosum
stratum granulosum
stratum lucidum (found only in thick skin)
stratum corneum
Stratum Basale
•
•
Only layer that undergoes mitosis
One layer of cells adjacent to the dermis
–
–
–
keratinocytes: most abundant; produce
keratin to waterproof the skin
melanocytes: cells with long, branched
cytoplasmic processes; produce a pigment
(black, brown, or yellow) that absorbs UV light
to prevent DNA damage, reducing some
forms of skin cancer
tactile cells: sense touch
Cells of the Stratum Basale
Figure 5.2
Melanocytes
Figure 5.4
Stratum Spinosum
• Several layers thick
• Daughter cells from the stratum basale
– differentiate into nondividing (may see a rare
mitotic cell), highly specialized keratinocyte
• Epidermal dendritic cells
– phagocytes that engulf invading pathogens
Cells of the Stratum Spinosum
Figure 5.2
Stratum Granulosum
• Three to five layers of keratinocytes
– cytoplasm fills with keratin filaments
– organelles begin to degrade
– fully keratinized cells are dead but strong and
water-insoluble
Stratum Granulosum Cells
Figure 5.2
Stratum Lucidum
• Thin, translucent region, two to three
layers thick
• Present only in thick skin such as sole of
feet and palms of hands
• Cells lack organelles, filled with eleidin
– transparent, intermediate product of keratin
maturation
Cells of the Stratum Lucidum
Figure 5.2
Stratum Corneum
•
•
•
Most superficial layer of epidermis
Thickness varies from a few to 30 layers
thick depending on location on the body
Comprised solely of dead keratinocytes
–
sloughed off by abrasion = dust
Cells of the Stratum Corneum
Figure 5.3
Epidermal Variation: Skin Color
Skin color is determined by three pigments:
• hemoglobin: blood pigment; causes
light complexions to look pink (or blue)
• melanin: pigment produced by
melanocytes; increases in people
exposed to more UV light
• carotene: yellow-orange pigment from
food that builds up in the skin
Abnormal Skin Colors
Epidermal Variation: Skin Markings
•
•
•
Nevus: localized overgrowth of melanocytes
– a.k.a. mole
Hemangioma: proliferation of blood vessels
– may disappear (strawberry) in childhood or
may persist (port-wine) through adulthood
Friction ridges: folds of epidermis/dermis on
fingers, palms, soles, and toes for grasping
– cause us to leave fingerprints
Fingerprints
Figure 5.5
The Dermis
•
•
Lies deep to the epidermis
Two layers of connective tissues:
–
–
Papillary: superficial
Reticular: deeper
• mainly collagen fibers
• contains blood vessels, glands, hair
follicles, nail roots, sensory nerve
endings, and smooth muscle
The Dermis
Figure 5.6
The Papillary Layer
• Directly below stratum basale cells of
epidermis
– dermal papillae and epidermal ridges
interlock, increasing the surface area
between epidermis and dermis
– dermal papillae contain capillaries that
supply nutrients to the avascular
epidermal cells
The Reticular Layer
• Forms majority of the dermis
• Comprised mainly of dense irregular
connective tissue with large bundles of
collagen fibers, blood vessels, glands, hair
follicles, and nerves
– collagen bundles help connect dermis to
underlying hypodermis
Lines of Cleavage
• Lines in the deep dermis formed by the
orientation of collagen bundles
– importance to surgeons: incisions across
these lines heal more slowly than incisions
along the lines
Lines of Cleavage
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
An incision
perpendicular to
cleavage lines may
gape and delay healing.
Figure 5.7
An incision parallel
to cleavage lines is more
likely to heal quickly and
not gape open.
Innervation
• Nerve fibers are present in dermis
– Functions:
• tactile (touch) receptors
• control blood flow
• control glandular secretion
Blood Supply
•
•
Epidermis: avascular
Dermis: contains blood vessels
–
important in controlling body temperature
• vasoconstriction: narrowing blood
vessels preserves core body heat
• vasodilation: widening blood vessels
releases body heat, lowering body
temperature
The Hypodermis
• A.K.A. subcutaneous layer
– deep to, not really part of, the integument
– areolar and adipose connective tissues
• Functions:
– protects underlying structures
– stores energy
– thermal insulation
Hypodermis (Subcutaneous Layer)
Figure 5.6
Epidermal Derivatives
•
Structures that grow from the epidermis:
– Nails
– Hairs
– Glands
Nails
• Derived from the stratum corneum
• Cells densely packed together filled with
parallel fibers of hard keratin
• The nail plate has a whitish free edge, a
pinkish nail body, and a nail root
• The nail body covers a layer of epidermis
called the nail bed
• The nail bed appears pink because of the
underlying capillaries
Nails
• Protective structures on digits
• Parts
– nail body: flat keratinized cells protecting
digit
– nail bed: live epidermal cells under nail body
– nail root: region hidden by cuticle
• nail matrix: thickened growing part of the nail bed
• lunula: white semilunar proximal area of nail body
caused by thickened underlying stratum basale
obscuring capillaries in dermis
Fingernail
Figure 5.8
Hair
•
•
Columns of keratinocytes growing from
follicles deep in dermis or hypodermis
Regions of a hair from deep to surface:
–
–
–
Hair bulb
Hair root
Hair shaft
Structure of a Hair
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Shaft
(beyond epidermis)
Root
Sebaceous
(oil) gland
Hair follicle
Arrector
pili muscle
Matrix
Figure 5.9
Hair bulb
Melanocyte
Hair papilla
(a)
Hair Structure
•
From deep to superficial
–
–
–
hair papilla: connective tissue, nerves, and blood
vessels below follicle that support the
keratinocytes
hair bulb: a swelling at bottom of follicle filled
with dividing keratinocytes; increase in hair
matrix causes hair growth
arrector pili: involuntary smooth muscle attached
to hair shaft; responds to emotional states (fear or
rage) and cold temperatures by contracting,
standing hair up, and producing “goose bumps”
Structure of a Hair
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Connective
tissue root
sheath
Cortex
Cuticle
External root
sheath
Internal root
sheath
Hair
bulb
Matrix
Hair papilla
LM 100x
Figure 5.9
(b)
© Biophoto Associates/Photo Researchers, Inc.
Functions of Hair
•
•
•
•
•
•
Protection
Heat retention
Facial expression
Sensory reception
Visual identification
Chemical signal dispersal
Skin Exocrine Glands
•
Two most common types:
–
–
•
sweat glands: produce watery solution
• merocrine and apocrine
sebaceous glands: produce oily
secretions
Two rarer types:
–
–
ceruminous glands: produce ear wax
mammary glands: produce milk
Sweat Glands
Figure 5.10
Merocrine Sweat Glands
• Simple coiled tubular glands that secrete into a
duct with a pore on skin’s surface
– secretion is 99% H2O, clear, and controlled by
nervous system
– numerous on forehead, palms, and soles
• Functions:
– Thermoregulation
– Secretion
– Protection
Apocrine Sweat Glands
• Simple coiled tubular glands that secrete into
hair follicles around nipples (areolae), armpits
(axillae), groin (pubic), and anus (anal)
– secretion is thick, cloudy, proteins and lipids
• leads to bacterial growth, causing body
odor in the above regions
Sebaceous Glands
• Secrete oily sebum into hair follicles
– lubricates hair and skin
– relatively inactive during childhood; sex
hormones at puberty cause secretions to
increase significantly