Ebola Contact Tracing
advertisement
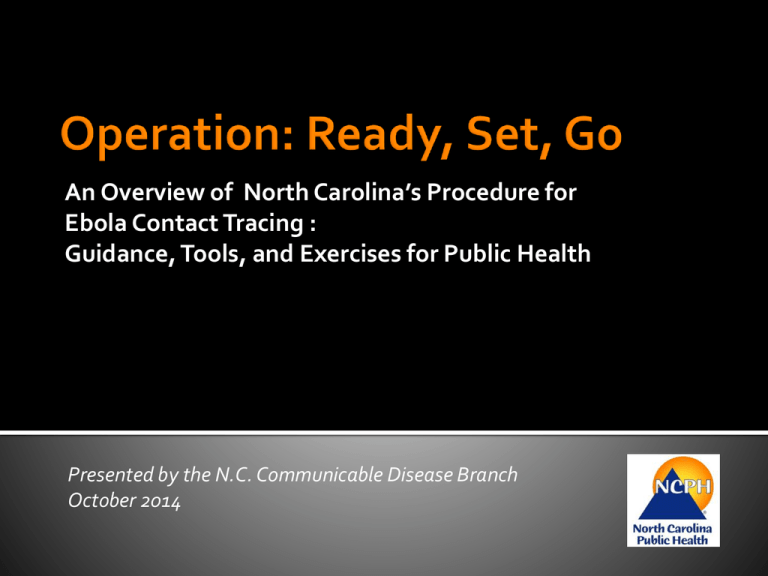
EBOLA CONTACT TRACING FOR LOCAL HEALTH DEPARTMENTS An Overview of North Carolina’s Procedure for Ebola Contact Tracing : Guidance, Tools, and Exercises for Public Health Presented by the N.C. Communicable Disease Branch October 2014 Use this next week to Get Ready: Acknowledge the critical role that contact tracing plays in interrupting disease transmission Assess your capacity to conduct a scalable Ebola contact tracing event Describe the process and locate the data collection data management tools Prepare for onsite state and federal assistance Exercise multiple tabletop exercises for Ebola contact tracing R – Review the Guidance E – Engage your Epi Team A – Assess your Capacity D – Designate your Tracers Y – Yes to Tabletop Exercises Deploy state team immediately for assistance with data management Epidemiologist Deploy state team for field investigations Nurse Consultant Disease Intervention Specialist Access to Risk Assessment Advisor Personal Readiness Kits Thermometers Prepare, Practice and Practice Know the Procedures Know the Tools Talk, Reassure, Support Travel in Pairs Do not touch Documents Table of Contents EZ Document ID -A B1 B2 B3 C D1 D2 D2-F D2-S D3 D3-F D3-S D4 D4-F D4-S Ebola Document Name N.C. Contact Tracing Webinar Presentations N.C. Contact Tracing Procedure N.C. Contact Listing Questionnaire- Part 1 N.C. Contact Listing Questionnaire- Part 2 N.C. Contact Listing Spreadsheet N.C. Contact Investigation Questionnaire N.C. Monitoring Instructions for the LHD N.C. Monitoring Instructions for the Contact N.C. Monitoring Instructions for the Contact (French) N.C. Monitoring Instructions for the Contact (Spanish) N.C. Guidance for the Contact Who Becomes Ill N.C. Guidance for the Contact Who Becomes Ill (French) N.C. Guidance for the Contact Who Becomes Ill (Spanish) N.C. Ebola Symptom Monitoring Log N.C. Ebola Symptom Monitoring Log (French) N.C. Ebola Symptom Monitoring Log (Spanish) Factsabout Ebola Ebola virus is not spread through Casual contact Air Water Foodgrownor legallypurchasedin theU.S. Howdoyouget theEbolavirus? 1. Identification and interviewing 2. Active monitoring a. Identify contacts by interviewing patient or other informants Monitor contacts with high- or low-risk exposures for 21 days following last exposure b. Interview all identified contacts to evaluate need for PH follow-up 3. Discharge Release on 22nd day following last exposure At ANY point in this process you may encounter contacts with symptoms of Ebola. You must know and be able to carry out your LHD procedure to safely respond to this situation. 1. Identification and interviewing a. Identify contacts by interviewing patient or other informants b. Interview all identified contacts to evaluate need for PH follow-up 1. Identification and interviewing a. Identify contacts by interviewing patient or other informants b. Interview all identified contacts to evaluate need for PH follow-up 1. Identification and interviewing a. Identify contacts by interviewing patient or other informants b. Interview all identified contacts to evaluate need for PH follow-up 1. Identification and interviewing a. Identify contacts by interviewing patient or other informants b. Interview all identified contacts to evaluate need for PH follow-up 2. Active monitoring Monitor contacts with high- or low-risk exposures for 21 days following last exposure 2. Active monitoring Monitor contacts with high- or low-risk exposures for 21 days following last exposure 2. Active monitoring Monitor contacts with high- or low-risk exposures for 21 days following last exposure 2. Active monitoring Monitor contacts with high- or low-risk exposures for 21 days following last exposure 3. Discharge Release on 22nd day following last exposure 1. Identification and interviewing 2. Active monitoring a. Identify contacts by interviewing patient or other informants Monitor contacts with high- or low-risk exposures for 21 days following last exposure b. Interview all identified contacts to evaluate need for PH follow-up 3. Discharge Release on 22nd day following last exposure 1. Every case and potential contact receives a unique ID EID EXXX 2. For each case a person may have been exposed to, a contact ID Number is created: Contact ID Number 1 NNNN-XXX 3. If any contact becomes a case they also receive an NC EDSS Event Number: Contact ID Number n NNNN-XXX Every potential contact will receive a minimum of two ID numbers: an EID and at least one contact ID number (a person may have multiple contact ID numbers if exposed to multiple cases). They will also have an NC EDSS event number if they become symptomatic. Contact tracing for our first case Name EID NC EDSS Event Contact ID Number Number John Snow E001 100905678 Edward Jenner E002 Louis Pasteur E003 100904567 5678-001 5678-002 Contact tracing for our second case Name EID Florence Nightingale E004 NC EDSS Event Number --- Contact ID Number 4567-001 Louis Pasteur --- 4567-002 E003 Documents Table of Contents EZ Document ID -A B1 B2 B3 C D1 D2 D2-F D2-S D3 D3-F D3-S D4 D4-F D4-S Ebola Document Name N.C. Contact Tracing Webinar Presentations N.C. Contact Tracing Procedure N.C. Contact Listing Questionnaire- Part 1 N.C. Contact Listing Questionnaire- Part 2 N.C. Contact Listing Spreadsheet N.C. Contact Investigation Questionnaire N.C. Monitoring Instructions for the LHD N.C. Monitoring Instructions for the Contact N.C. Monitoring Instructions for the Contact (French) N.C. Monitoring Instructions for the Contact (Spanish) N.C. Guidance for the Contact Who Becomes Ill N.C. Guidance for the Contact Who Becomes Ill (French) N.C. Guidance for the Contact Who Becomes Ill (Spanish) N.C. Ebola Symptom Monitoring Log N.C. Ebola Symptom Monitoring Log (French) N.C. Ebola Symptom Monitoring Log (Spanish) Documents Table of Contents Documents are available online The CDB webpage: http://epi.publichealth.nc.gov/cd/diseases/hemorrhagic.html OR CD Manual: http://epi.publichealth.nc.gov/cd/lhds/manuals/cd/reportable_diseases.html And More… • Survey Monkey Evaluation • Onsite Instruction for Tracers Kathy Dail, RN MEd Heather Dubendris, MSPH Kristin Sullivan, MPH Rob Pace, BGS Reed Underhill, BA North Carolina Division of Public Health Communicable Disease Branch Bhavini Patel Murthy, MD, MPH Preventive Medicine Resident University of North Carolina at Chapel Hill Neil Chandra Murthy, MD, MPH Emergency Medicine Resident Duke University Medical Center