Neuro Assessment
advertisement
Neurological Assessment At the end of this self study the participant will: 1. Describe the neuro nursing assessment 2. List 5 abnormal findings in a neuro assessment 3. List 3 early signs which would indicate the patient is worsening 4. List 3 late signs of neurological depression. 1 Neurological Assessment Level of Consciousness Most sensitive indicator of neurological change Measurement of a person's arousability and responsiveness to stimuli from the environment (not accuracy of response to questions) Impairments to Assessment Trauma Alcohol Insulin Epilepsy Psych Infection Poison Opiates Shock/Stroke 2 Level of Consciousness Patient’s level of awareness - don’t confuse with orientation Awake - interactive Lethargic - sleepy, drowsy, rousable/responsive Stuporous - arousable with stimuli, resists arousal Obtunded - cannot maintain arousal without repeated stimuli, moans/groans to stimuli Comatose - non interactive with surroundings Orientation (appropriateness) Person, place, time, situation 3 Glascow Coma Scale • Assesses level of consciousness • Look for patients’ best responses • Total the numbers for documentation • Restrictions: – If eyes swollen closed, use “C” instead of number (maximum 11C) – For artificial airway, use “T” instead of number (maximum 10T) 4 Parameter Score Response Eye Opening 4 3 2 4 C Spontaneous To Voice To Pain No Response Closed by swelling Best Verbal Response 5 4 3 2 1 T Oriented Confused Inappropriate Words Incomprehensible sounds* No response or Intubated Artificial Airway Best Motor Response 6 5 4 3 2 1 Follows commands Purposeful, localizes Withdraws Abnormal Flexion ** Abnormal Extension** No response Total 3/15-15/15 Pupillary Response PERRLA: pupils equal, round and reactive to light and accommodation Pupil size Response to light Brisk Sluggish Non-reactive/fixed 5 Pupillary Response Accommodation have patient focus on your finger and move finger towards their nose Pupils should constrict and eyes should cross Alteration Changes seen on which side? Hippus: spasmodic, rhythmic but irregular dilating and contracting pupillary movement 6 Reflexes Corneal Reflex Blink reflex To assess, touch cornea with tip of cotton, instill eye drop, touch lashes Gag Reflex Airway protection mechanism Neck injury/surgery Aspiration risk Voice changes Volume changes 7 Extremity Assessment Strength Sensory Pinprick Hand grasps Arm drift 8 Touch Warm/cold Foot flexion Compare right to left Assess with resistance Neurological Assessment Motor Assessment Response to stimuli - Normal vs Abnormal Abnormal Posturing: Decorticate posturing/flexor posturing Decerebrate posturing/extensor posturing 9 When is your patient in trouble? • Behavior changes first – If normally quiet, may get restless or vocal – If normally boisterous, may get quiet • Speech next – Slurring, difficulty forming words • Orientation next – Oriented x4 on admission, starts forgetting what you’ve said is going on – Oriented x3 • Arousability next – Drowsiness but may respond to stimuli – Glascow Coma Scale changes 10 Early signs your patient is in trouble Early signs: 1. Decreasing LOC: needs more stimulus to display same responses 2. Motor: Subtle weakness on one side, pronator drift. 3. Pupils: Sluggish reaction; unilateral hippus; an ovoid shape; any irregularity that is unusual for the patient. 4. VS: Not reliable at this point; may have cheynestokes respirations, but is dependent upon where the lesion is located in the brain. 11 Late signs your patient is in trouble 1. LOC: Unarousable. 2. Motor: Dense weakness on a side; worsening responses to painful stimuli; posturing; then no response. 3. Pupils: One “blown” pupil; then both fixed and dilated. 4. VS: Cushing’s triad: – widening pulse pressure (increased SBP) – profoundly slow pulse rate, – abnormal respirations. 12 Tips for accurate neuro assessments • Always use the same structure for your assessment – Head to toe • Always compare right to left – Asymmetry is abnormal • Take your time. Patients’ response times vary with age, history, medications, and other factors • If a family member tells you something is wrong, investigate – Level of consciousness is the most sensitive indicator of neuro status – Family may pick up on something staff may not abcdefghi see as abnormal 13 14

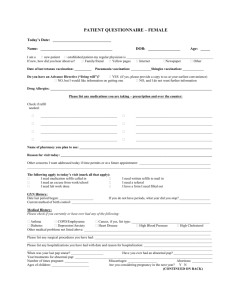

![afl_mat[1]](http://s2.studylib.net/store/data/005387843_1-8371eaaba182de7da429cb4369cd28fc-300x300.png)