to a PowerPoint presentation on a qualitative study
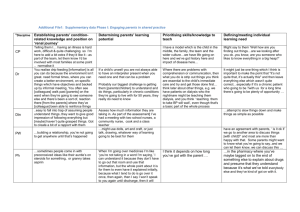
advertisement

Understanding the older person with cancer: a qualitative study of two wards Tentative findings Antonia Lannie, PhD student, Supervisors Prof. R. Barbour & Dr.J.Corlett Findings Ward as a ‘half way house’ ‘Etiquette’ ‘Emotion work’ ‘Hope’ The ward as a ‘Half Way House’ I think hospitals are a great place if you need them. I needed them. Not only me but my wife did as well. That’s why I’ve always had that attitude; hospitals are a great place if you need them and I’ve needed them …I would say it’s a safe place. (Male Patient) Giving them company to reflect on life that is there. (Health Care Professional) The ward as a ‘Half Way House’ When am I going home? because regardless of how well off you are and how much attention you get, the psychological state of a person who is ill and who thinks about this illness is, ‘Will I be safer to be here, or be in my own house?’ And ironically you always feel safer going to hospital and when you are here you want to go home. (Male Patient) It’s a barrier they don’t want you to cross-they are quite happy to be independent, but when they do need you they still don’t want you to do it, but you need to do it. (Senior Staff Nurse) ‘Etiquette’ –relationships I feel they could inform you more. May be there are certain things etiquette, or whatever you call it, stops them from saying too much I said to one of the doctors, ‘What’s your opinion, never mind your professional opinion, what’s your opinion?’ And he said, ‘I’m not allowed to air opinions (Male Patient) … but she is a very funny person. Her vibes, I don’t know how to word this to be sociable. (She often says ) .‘Don’t worry about it, don’t worry about it.’ But I do worry about it. It is a very funny thing to say to a patient. (Female patient). I think it’s because it’s their (relating to Doctors ) general practice and things like that. They have to be good whether they want to be good or not they’ve got to bite their tongue and be good. (Female patient). ‘Etiquette’ – Professional and personal I always remember meeting a junior doctor once and she said, ‘that’s terrible,’ you know about this patient, ‘How could they, how must their wife be feeling and how must their mum and dad be feeling?’ and it was like, ‘Whoa, whoa, whoa, you have to stop right there, you can’t think like that.’ And you have to stop, that is the challenge…there some people that do get involved but I have never been like that, never, because I just don’t, it’s not that I don’t think it is professional, I am not saying that but I just think it is a coping mechanism is not to get too involved. (Senior female Staff Nurse) here it is different because you are forming different relationships with your patients and also because they are younger as well you empathise with them… maybe it’s because I am getting older as well, I am a bit more emotional as I get older (Researchers emphasis) .(Junior female staff nurse) ‘Emotion Work’ -Patients dealing with others’ emotions …they feel for their family as well as themselves. (Health Care professional) They (his family) will look after her (his wife), no doubt about it….you won’t need to go to the undertaker and break her heart or anything because everything has been done (Male Patient) Emotion work; Dealing with Professionals’ emotions ‘Don’t worry about it.' (Researcher's emphasis) But how the hell could you worry, you have to worry about it. I’m worrying about what’s going to happen to me and she’ll go, ‘Don’t worry about it.’ That’s the kind of, now that’s not nursing care, it’s not really. They need to say things better than that; she needs to put it in a better way. It’s not for me to say. (Female patient) ‘Hope’ And to give people hope, you try to give people hope but you don’t want them to be too ‘well this is going to cure me’. It is finding that balance. You don’t want them to think that after this I’ll be cured. It is a balancing act. (Senior Staff Nurse) Some people grab hold of what you are saying with two hands (Senior Nurse CNS) The non toxic side of the treatment now, is massive. (Junior Staff Nurse) ‘Hope’ - The Clinical and Social Construction of Dying Well, put it this way anybody that’s got this I think they would think the same. I had a neighbour, he died, and he went through the same thing as I have. He went through chemo, he went through this and was tired and all the rest of it. Well I’m going through the same problems and he died because he had enough, had enough. Well I think I’m going the same way, I’ve had enough, so I know I am going but when I don’t know. But hopefully I don’t suffer at the end (Researcher’s emphasis). (Retired nurse and patient) Questions Do you think it’s helpful to think of the ‘ward as a half way house’ ? Is ‘etiquette’ helpful or a barrier ? Do you recognise any of these patterns of ‘emotion work’ ? How do we think about the use of ‘hope’ in our clinical practice ?