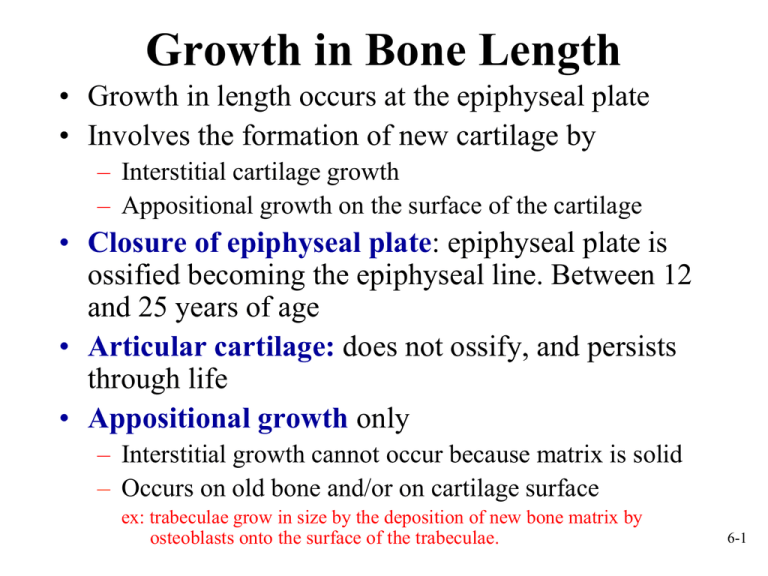
Growth in Bone Length
• Growth in length occurs at the epiphyseal plate
• Involves the formation of new cartilage by
– Interstitial cartilage growth
– Appositional growth on the surface of the cartilage
• Closure of epiphyseal plate: epiphyseal plate is
ossified becoming the epiphyseal line. Between 12
and 25 years of age
• Articular cartilage: does not ossify, and persists
through life
• Appositional growth only
– Interstitial growth cannot occur because matrix is solid
– Occurs on old bone and/or on cartilage surface
ex: trabeculae grow in size by the deposition of new bone matrix by
osteoblasts onto the surface of the trabeculae.
6-1
Zones of the Epiphyseal Plate
6-2
Growth in Bone Length
6-3
Growth at Articular Cartilage
• Increases size of bones with no epiphyses: e.g.,
short bones
• Chondrocytes near the surface of the articular
cartilage similar to those in zone of resting cartilage
• The process of growth in articular cartilage is
similar to that occurring in the epiphyseal plate,
except that the chondrocyte columns are not as
obvious.
• When epiphyses reach their full size, the growth of
cartilage & its replacement by bone cease.
• However, articular cartilage persists throughout life
& does not become ossified as does epiphyseal
plate.
6-4
Fracture of the Epiphyseal Plate
6-5
Growth in Bone Width
6-6
Factors Affecting Bone Growth
• Size and shape of a bone determined genetically but can be
modified and influenced by nutrition and hormones
• Nutrition
– Lack of calcium, protein and other nutrients during growth and
development can cause bones to be small
– Vitamin D
• Necessary for absorption of calcium from intestines
• Can be eaten or manufactured in the body
• Rickets: lack of vitamin D during childhood (bowed bones)
• Osteomalacia: lack of vitamin D during adulthood leading to
softening of bones
– Vitamin C
• Necessary for collagen synthesis by osteoblasts
• Scurvy: deficiency of vitamin C (causes ulceration & hemorrhage in
body)
• Lack of vitamin C also causes wounds not to heal (because requires
collagen synthesis), teeth to fall out (because ligaments that hold them in
place break down)
6-7
Factors Affecting Bone Growth
(cont.)
• Hormones
– Growth hormone from anterior pituitary. Stimulates
interstitial cartilage growth and appositional bone
growth
– Thyroid hormone required for growth of all tissues
– Sex hormones such as estrogen and testosterone
• Cause growth at puberty, but also cause closure of the
epiphyseal plates and the cessation of growth
6-8
Bone Remodeling
• Converts woven bone into lamellar bone
• Caused by migration of Basic
Multicellular Units (BMU)
– Groups of osteoclasts and osteoblasts that
remodel bones
• Involved in bone growth, changes in bone
shape, adjustments in bone due to stress,
bone repair, and Ca ion regulation
• Relative thickness of bone changes as
bone grows. Bone constantly removed by
osteoclasts and new bone formed by
osteoblasts.
• Formation of new osteons in compact
bone
– Osteoclasts enter the osteon from blood in
the central canal and internally remove
lamellae. Osteoblasts replace bone
– Osteoclasts remove bone from the
6-9
exterior and the bone is rebuilt
Bone Repair
1.
Hematoma formation. Localized mass of blood released from blood vessels
(damaged from fracture) but confined within an organ or space. Clot formation
(consists of fibrous proteins that stop the bleeding).
2.
Callus formation. Callus: mass of tissue that forms at a fracture site and
connects the broken ends of the bone.
- Internal- blood vessels grow into clot in hematoma (several days after fracture).
• Macrophages clean up debris, osteoclasts break down dead tissue,
fibroblasts produce collagen and granulation tissue.
• Chondroblasts from osteochondral progenitor cells of periosteum and
endosteum produce cartilage within the collagen.
• Osteoblasts invade. New bone is
formed.
- External- collar around opposing
ends. Periosteal osteochondral
progenitor cells osteoblasts
and chondroblasts. Bone/cartilage
collar stabilizes two pieces.
6-10
Bone Repair, cont.
3.
4.
Callus ossification. Callus replaced by woven,
cancellous bone through endochondral ossification.
Bone remodeling. Replacement of cancellous bone and
damaged material by compact bone. Sculpting of site by
osteoclasts
6-11
Calcium Homeostasis
• Bone is major storage site for calcium
• The level of calcium in the blood depends
upon movement of calcium into or out of
bone.
– Calcium enters bone when osteoblasts create
new bone; calcium leaves bone when
osteoclasts break down bone
– Two hormones control blood calcium levelsparathyroid hormone (produced by parathyroid gland---blood calcium decreases then secretion of PTH increases which
increases # of osteoclasts) and calcitonin ( produced by
thyroid gland----decreases osteoclast activity
6-12
Calcium Homeostasis
6-13
Effects of Aging on Skeletal
System
• Bone matrix decreases. More brittle due to lack of collagen;
but also less hydroxyapatite.
• Bone mass decreases. Highest around 30. Men denser due to
testosterone and greater weight. African Americans and
Hispanics have higher bone masses than Caucasians and
Asians. Rate of bone loss increases 10 fold after menopause.
Cancellous bone lost first, then compact.
• Increased bone fractures
• Bone loss causes deformity, loss of height, pain, stiffness
– Stooped posture
– Loss of teeth
6-14
Bone Fractures
• Open (compound)- bone break with
open wound. Bone may be sticking
out of wound.
• Closed (simple)- Skin not perforated.
• Incomplete- doesn’t extend across the
bone. Complete- does
• Greenstick: incomplete fracture that
occurs on the convex side of the curve
of a bone
• Hairline: incomplete where two
sections of bone do not separate.
Common in skull fractures
• Comminuted fractures: complete with
break into more than two pieces
6-15
Bone Fractures, cont.
• Impacted fractures: one
fragment is driven into the
cancellous portion of the
other fragment.
• Classified on basis of
direction of fracture
• Linear
• Transverse
• Spiral
• Oblique
• Dentate: rough, toothed,
broken ends
• Stellate radiating out from a
central point.
6-16