Slide 1
advertisement

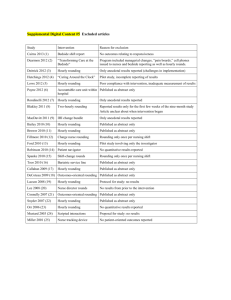
Hourly Rounding: A systematic approach to patient safety Paula Anton, MS. RN, CRRN, ACNS-BC, Michelle Fernamberg, MHA, BSN, RN, CRRN, Leah Shever, PhD, RN, Mary L. Parker, MS, RN, 6A Professional Practice Council 6A Acute Rehabilitation Nursing, University of Michigan, Ann Arbor, MI Purpose Hourly rounding has been demonstrated to improve outcomes in acute care. Over the past 4 years, various units at University of Michigan Hospitals have implemented hourly rounding processes. Units have had varied results and difficulty sustaining those results and Hourly Rounding in practice. The purpose of this project was to standardize an evidence-based, patient-focused intentional surveillance of the patient that contributes to: • optimal patient outcomes • improved patient satisfaction • decreased call light use • decreased falls Synthesis Studies describe Hourly Rounding as a group of interventions that improves call light use, patient satisfaction, and safety.2, 5, 6 Recent studies describe these results in multiple settings. 3, 4, 5, 9. Activities of the nurse during rounds vary by study, but some reviews are beginning to identify common trends in activities that make the most impact. 4, 9 Toileting at specific times is known to decrease falls in elderly and patients on diuretics. 1, 7, 10 Implementation Strategies The Professional Practice Council was involved in the decision to implement Hourly Rounding. They participated in education of peers on the process, and were embedded in planning the strategy for implementation. Staff were educated on the process for rounding and how the process and outcomes would be measured. 4, 6 Leaders provided feedback to staff regularly. To determine how well the process is implemented on the unit, following data sources were monitored: • Leader Rounding in which unit leaders round on staff and patients to ask them directly about the Hourly Rounding process. 2, 8 • Chart audits for documentation of pain/comfort, toileting and activity/positioning. Evaluation Outcome measures included call light data, falls and patient satisfaction with nursing care and response to call lights. Findings were mixed. Call light use did not change in response to rounding. The patients reported process was well adhered to, with nurses providing the interventions as prescribed. Patient satisfaction improved. Evaluation Initially falls decreased, but later an increase in falls prompted additional chart audits. Results suggested that toileting may not have been being done pro-actively, in spite of patient comments that it was. Significance While Hourly Rounding is well established as a helpful set of interventions for improving patient outcomes, it is clear that leadership commitment to monitoring staff compliance with the process is needed to hardwire the practice.3, 4, 8 It is possible that the complexity of such a grouping of interventions results in difficulty keeping the practice going, and evidence from this project indicate that pro-active toileting may be the most important intervention. References Change A pilot was conducted on 6A in which, at prescribed intervals, the nursing staff performed activities that focus on four basic areas of nursing care: • Pain and comfort • Safety and environment • Positioning and activity • Pro-active toileting Specific language was used to systematically convey activities to the patients. 1. Asplund, R. (2007). Pharmacotherapy for nocturia in the elderly patient. Drugs & Aging, 24(4), 325-343. 2. Bourgault, A.M., King, M.M., Hart, P., Campbell, M.J., Swartz, S., & Lou, M. (2008). Circle of excellence. Nursing Management, 39(11), 18-25 3. Gardner, G., et.al (2009). Measuring the effect of pt comfort rds on practice environ & pt satisf: A pilot study. Internatl Jrnl of Nrsg Practice, 15: 287-293. 4. Halm, M. (2009). Hourly rounds: What does the evidence indicate? American Journal of Critical Care, 18(6), 581584. 5. McCartney, P. (2009). Hourly rounds: An evidence-based practice. MCN: The American Journal of Maternal Child Nursing, 34(5), 327. 6. Meade, C., Bursell, A., & Ketelsen, L. (2006). Effects of nursing rounds on patients’ call light use, satisfaction, and safety. American Journal of Nursing, 106(9), 58-70. 7. Morgan, C., Endoza, N., Paradiso, C., McNamara, M., Mcguire, M. (2008). Enhanced toileting program decreases incontinence in long term care. The Joint Commission Journal on Quality and Patient Safety, 34(4) 206-208. 8. Studer, Q. 2003. Hardwiring Excellence. (pp. 148-153) Gulf Breeze, FL: Fire Starter Publishing 9. Weisgram, B. & Raymond, S. (2008) Using evidence-based nursing rounds to improve patient outcomes. MedSurg Nursing 17 (6) 429-430 10. Woolcott, M., Richardson, K., Wiens, M., Patel, B., Marin, J., Khan, K., & Marra, C. (2009). Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Archives of Internal Medicine, 168(21), 1952-1959.