pancreatic secretion
advertisement

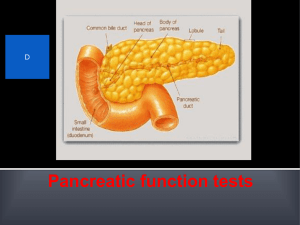
EXOCRINE PANCREATIC SECRETION OBJECTIVES The student should be able to: • Discuss pancreatic exocrine secretion and composition. • Enlist pancreatic enzymes and their importance • Describe steatorrhea. • Explain the mechanism of pancreatic juice secretion. • Describe the regulation of pancreatic exocrine secretion hormonal and neural. PANCREATIC SECRETION • When food enters the duodenum, it is mixed with pancreatic secretion and bile [pancreas and liver are accessory digestive organs]. • Pancreas is elongated gland lies behind and below the stomach. • It has exocrine and endocrine secretions. • Exocrine Pancreas secretes pancreatic juice. PANCREATIC SECRETION • Pancreas has acini and ducts: 1) Pancreatic acinar cells secrete digestive enzymes. 1) Pancreatic duct cells secrete [aqueous] watery alkaline fluid rich in NaHCO3 Pancreatic Juice Exocrine pancreatic secretion: • Volume = 1-2 L / day. • pH = approximately 8 (alkaline). • Osmolarity = isotonic. • It has Water, Cations (Na+, K+, Ca+2), Anions (HCO3, Cl-, HPO4) & Digestive enzymes. Types of exocrine pancreatic secretion Aqueous alkaline juice Enzymatic juice Secreted by duct cells. Secreted by acinar cells. Large in volume, rich in bicarbonate. Small in volume, rich in enzymes. Stimulated by Secretin. Inhibited by Sympathetic. Stimulated by CCK & vagus. 1) Pancreatic Enzymes: • Stored in zymogen granules after they are produced. • Released by exocytosis as needed. • Pancreatic enzymes are important because they can completely digest food, in absence of all other digestive secretions. • Pancreatic Acinar Cells Secrete Three Types of Pancreatic Enzymes: i. Proteolytic enzymes for protein digestion. ii. Pancreatic amylase for carbohydrate digestion. iii. Pancreatic Lipolytic for fat digestion. (i) Pancreatic Proteolytic Enzymes: • Major Proteolytic Enzymes are: 1- Trypsinogen. 2- Chymotrypsinogen. 3- Procarboxypeptidase. • They are secreted in inactive forms. • Proteolytic Enzymes attack different peptide linkages. • End result is formation of small peptide chains and amino acids. Activation of Pancreatic Proteolytic Enzymes • When Trypsinogen is secreted into duodenal lumen, it is activated to its active form Trypsin by Enterokinase (=Enteropeptidase) which is an intestinal enzyme embedded in mucus membrane of duodenal mucosa. • Once Trypsin is formed, it activates more Trypsinogen [autocatalytic]. • Chymotrypsinogen & Procarboxypeptidase are converted to active forms by Trypsin in duodenal lumen. • Initially, intestinal enterokinase is needed to form trypsin. Once trypsin is formed, it carries out other processes. (ii). Pancreatic Amylase For Carbohydrate Digestion: • It causes conversion of polysaccharides into disaccharide maltose. • It is secreted in the Active form as there is no risk for auto digestion of pancreas. (iii) Pancreatic Lipase for Fat Digestion: • It is the most important enzyme secreted throughout digestive system that can digest fat. • In human, there are insignificant amounts of Lingual Lipase & Gastric Lipase. • Pancreatic lipase can hydrolyze dietary triglycerides into Monoglyceride & Free fatty acids, which are absorbed in small intestine. • It is secreted in the Active form as there is no risk for auto digestion of pancreas. 2- Pancreatic Aqueous Alkaline Fluid: As highly acidic Gastric contents are emptied into duodenal lumen, this acidic Chyme must be neutralized quickly in duodenal lumen, Why? 1- To allow the functioning of pancreatic enzymes [they work in neutral or slightly alkaline medium]. NaHCO3 in pancreatic fluid neutralizes the acidic Chyme. 2- To prevent damage to duodenal mucosa. CONTROL OF PANCREATIC EXOCRINE SECRETION 1- Nervous: Vagal stimulation enzymatic secretion from acini (little contribution during cephalic phase). 2- Hormonal: Secretin aqueous secretion from duct. CCK enzymatic secretion from acini. When Chyme enters the duodenum, secretin & CCK [Entrogastrones] are released in response to Chyme. Structure Site Stimuli Cholecystokinin Secretin 22 A.A 27 A.A Upper part of small intestine (deudenum). HCL that passes to Polypeptides & AA duodenum with Fats & F.A. in duodenum. decrease its pH. Functions: On Stomach: Inhibition of gastric functions On Intestine: Motility & enzymes secretion. Mucus secretion. On Pancreas: Secretion of enzymes. Evacuation of bile (cholagogue) Secretion of alkaline juice. Secretion of NaHco3 (choleretic) + ve Feedback between CCK & A.A as CCK digestion of protein production of amino acids CCK - ve Feedback as Hcl release of secretin Hcl secretion from the stomach. On Bile: Control: Pancreatic Insufficiency • When pancreatic enzymes are deficient, digestion of food is incomplete. • As pancreatic lipase is the significant source for fat digestion, its deficiency results in maldigestion of fats, it is called steatorrhea (increased undigested fat in feces). • Up to 60 – 70% of fat taken may be excreted in feces. • Digestion of protein and carbohydrate are impaired to a lesser degree because salivary, gastric and small intestinal enzymes contribute to their digestion. Steatorrhea • Definition: It is the presence of excess fat in feces. Stools may also float due to excess lipid, have an oily appearance and can be especially foul-smelling. • Possible causes: 1- lack of bile acids (due to liver damage). 2- Gall bladder removal (cholecystectomy). 3- Defects in Pancreatic enzymes e.g. Lipase 4- Malabsorption e.g. in Inflammatory bowel disease. 5- Exocrine pancreatic insufficiency & Pancreatitis. • Treatment: correction of the underlying cause, as well as digestive enzyme supplements.