Milestones - EM Milestones Wiki
advertisement
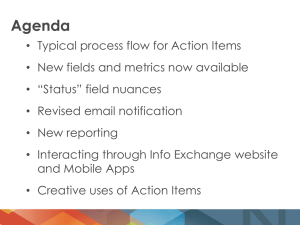
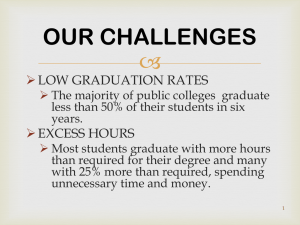
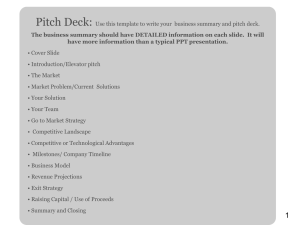
EM Milestones and Resource Development CORD 2013 EM Milestones and Resource Development • Putting Competency Based Education into Practice – Doug • Intro to the EM Milestones Wiki – Joint Milestones Task Force • When you get home, get on the Wiki and see what works for you • Not a finished product but a starting point Douglas Char, MD FACEP FAAEM CORD Academic Assembly March 2013 We are at a tipping point in competency-based medical education (CBME) — and it’s only taken 40 years since the competency conversation first appeared in the medical literature! In case you were not aboard the CBME train as it left the station, this concept is an integrated framework for education, in which specific behavioral outcomes (competencies) drive both medical school curricula and individual advancement, rather than the current driving forces of time (four years of medical school) and process (clerkships of specific length). Carol Aschenbrener – Chief Medical Officer, AAMC http://wingofzock.org/2012/09/25/competency-based-medical-education-the-time-is-now/ Traditional medical education presumes that all students are ready to graduate once they have completed a set number of years of study and passed the required assessments, There is a growing interest in tailoring the length as well as the content of medical education to individual aptitudes. “People learn in different ways and at different speeds,” “As early as 1932, reports emerged saying that it is not enough to stuff students’ heads with information Stakeholder no longer accepting residents as independent actors, they expect physicians to function as leaders and participants in team-oriented care. https://www.aamc.org/newsroom/reporter/april11/184286/competency-based_medical_education.html It is a curricular concept designed to provide the skills physicians need, rather than solely a large, prefabricated collection of knowledge. AThe medical school or residency program using scientific competency-based approach still includes competency-based medical education defines a set of knowledge, but in the broader context of a physician’s skills or competencies based societal and patient tasks as aon healer. needs, such as medical knowledge, patient care, or communications approaches, and then develops ways to teach that content across a range of courses and settings. https://www.aamc.org/newsroom/reporter/april11/184286/competency-based_medical_education.html We are wrestling with it just like everyone else. The challenge is not so much accepting the concept, which we think is great, but figuring out how to make it work. Where do we teach? How do we evaluate performance? How do we remediate students who have not met requirements?” Thomas Pellegrino - EVMS How to define competencies, and how to assess performance are perhaps the two most significant concerns about competency-based medical education. Peter Katsufrakis – NBME “we’ve been wrestling with this question for decades,” M. Brownell Anderson - AAMC Implementing competency-based training in postgraduate medical education poses many challenges. Making this transition requires change at virtually all levels of postgraduate training. Key components of this change include; Development of valid and reliable assessment tools such as work-based assessment using direct observation, Frequent formative feedback Learner self-directed assessment; Active involvement of the learner in the educational process; Intensive faculty development that addresses curricular design and the assessment of competency Iobst. Teach Med 2010; 32: 651–656 Bloom’s Taxonomy 1956 Anderson’s revision 2000 Cognitive (Knowledge) Affective (Attitude) Psychomotor (Skills) Remembering: can the student define, duplicate, list, memorize, recall, repeat, recall or remember the information? reproduce state Understanding: can the student explain ideas or concepts? classify, describe, discuss, explain, identify, locate, recognize, report, select, translate, paraphrase Applying: can the student use the information in a new way? choose, demonstrate, dramatize, employ, illustrate, interpret, operate, schedule, sketch, solve, use, write. Analyzing: can the student appraise, compare, contrast, criticize, differentiate, distinguish between the different discriminate, distinguish, examine, experiment, parts? question, test. Evaluating: can the student justify a appraise, argue, defend, judge, select, support, value, stand or decision? evaluate Creating: can the student create new assemble, construct, create, design, develop, formulate, product or point of view? write • Final milestones will provide meaningful data on the performance that graduates must achieve before entering unsupervised practice (graduate) • Initial milestones for entering residents will add a performance- based vocabulary to conversations with medical schools about graduates’ preparedness for supervised practice (residency) Norcini BMJ 2003:326(5):753-755 Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990:S63-7. Many people argue that this statement is incorrect and that the curriculum is the key in any clinical course. In reality, students feel overloaded by work and respond by studying only for the parts of the course that are assessed. To promote learning, assessment should be educational and formative—students should learn from tests and receive feedback on which to build their knowledge and skills Pragmatically, assessment is the most appropriate engine on which to harness the curriculum. V Wass. Lancet 2001; 357: 945–49 Trained Observers Common understanding of expectations Sensitive “eye” to key elements Consistent evaluation of a given level of performance Minimum number of quality observations Assessment based on 7-9 observations felt to be valid and reliable Interpreter/Synthesizer Experts Clinical Competency Committee Numbers produce range restriction Narratives are easily understood by faculty and produce data without range restriction Natural to how we teach and provide feedback Goalis to create verbal pictures 4 cm laceration right arm vs Danger here is that rather than engaging a total practicum to which other forms of learning discourse bring their insights, a limited professional education is based upon an inappropriate epistemology of competency Tendency to limit the reflection, intuition, experience and higher order competence necessary for expert, holistic or well developed practice Martin Talbot, Med Educ 2004; 38: 587–592 If your are feeling overwhelmed and confused by all this new jargon – you are not alone Your faculty are looking to you for answers! Nobody has all the answers so stop waiting for the Holy Grail? Better to join the legion of PDs working to define it There is no way to sort out the milestones without getting “dirty” – expect to make mistakes Assessment is suppose to drive curriculum (this is a game changer) Resistance if futile, give in and drink the kool aid Reduce your stress, it’s going to happen! Intro to EM Milestones Wiki Kevin Biese, MD, MAT EM Milestones Wiki JMTF – Work so far • • • • • Intro to the Wiki – Christina Care Based Milestones – Moshe Systems Based Milestones – Mary Jo Procedural Milestones – Jenna Milestones Workbook - Rodney Intro to Wiki Resources Christina Shenvi, MD, PhD WiiFM But ultimately, check back to… Accessing the wiki • Emmilestones.pbworks.org • You do not need a login • We hope this will be a helpful resource JMTF – Care-Based Milestones Moshe Weizberg, MD, FACEP THANK YOU • Committee • Nestor Rodriguez • Jason Seamon EVALUATIONS • How do you want to divide your milestones • What do you want your evaluation questions to look like • How do you label each level • Where do you want your comment boxes HOW DO YOU WANT TO DIVIDE YOUR MILESTONES • • • • All milestones on every evaluation Divide among various rotations Divide among faculty Divide by day of the month • Hit all core competencies • CCCs evaluate all milestones based on evals PRO’S AND CON’S PRO’s CON’s All milestones on every evaluation Lots of data Most information Very long evaluations Faculty compliance? Realistic? Divide among various rotations Select milestones that relate to that rotation Have to match up the right milestones to the right rotations/evaluators Divide among faculty Different faculty members become experts in evaluating their milestones Those faculty won’t have input on other milestones Divide by day of the month Hit every milestone every block Avoid lengthy evals Logistically challenging Hit or miss WHAT DO YOU WANT YOUR EVALS TO LOOK LIKE • Yes/No/N/A • Mix up elements from various milestones • Mirror the milestone pages PRO’S AND CON’S PRO’s CON’s Yes/No/N/A More accurate Better info on each element Many more questions Harder to feed into CCCs Mix up elements from various milestones Probably most accurate Very difficult to set up Very difficult to analyze May be confusing for faculty Mirror the milestone pages Easier Less questions Feeds cleanly into CCCs Resident hits some elements and not others Very wordy for faculty to read ?less accurate LESSONS LEARNED • • • • Many faculty gave all residents level 5 Faculty bias based on label of each level (PGY) Faculty education Resident education JMTF - Systems-Based Milestones Mary Jo Wagner, MD JMTF: Procedural Milestones Jenna Fredette, MD Christiana Health Care System jfredette@christianacare.org Progress So Far • Early Stages: Emails exchanged, surveys completed, one conference call good position for new members! • None the less we have created an agenda for moving forward in 2013 Challenges with Procedural Milestones • Achieving a Level 4/5 in a Procedural Milestone does not necessarily prove procedural proficiency Challenges with Procedural Milestones • Milestones addresses the following – – – – – – General Approach to Procedures Airway Management Vascular Access Focused Ultrasound Wound Management Anesthesia/Sedation • We perform and require proficiency in many more areas than this Current Agenda Moving Forward • Collect institutional checklists and come up with set of standardized procedural checklists • Add milestone language to the checklists when appropriate • Determine the best way to evaluate each of the milestones (?procedural shift cards, SDOTs, SIM labs…) • Welcome new ideas and input!! • JMTF Procedural Milestones Wiki JMTF - Milestone Workbook Rodney Omron, MD, MPH Structure: 2011 ABEM Model Content • • • • • • • • • • • • • • • • • • • • SIGNS, SYMPTOMS, AND PRESENTATIONS ABDOMINAL AND GASTROINTESTINAL DISORDERS CARDIOVASCULAR DISORDERS CUTANEOUS DISORDERS ENDOCRINE, METABOLIC, AND NUTRITIONAL DISORDERS ENVIRONMENTAL DISORDERS HEAD, EAR, EYE, NOSE, THROAT DISORDERS HEMATOLOGIC DISORDERS IMMUNE SYSTEM DISORDERS SYSTEMIC INFECTIOUS DISORDERS MUSCULOSKELETAL DISORDERS (NONTRAUMATIC) NERVOUS SYSTEM DISORDERS OBSTETRICS AND GYNECOLOGY PSYCHOBEHAVIORAL DISORDERS RENAL AND UROGENITAL DISORDERS THORACIC-RESPIRATORY DISORDERS TOICOLOGIC DISORDERS TRAUMATIC DISORDERS Procedures and skills integral to the practice of EMergency medicine other core competencies of the Practice of Emergency Medicine Validated Education Tools Contribute your validated educational research Thank you!!!! • Just a start • Joint Milestones Task Force – 11:30 – 1:00 Today Spruce Room – Keep the great work coming