Incorporating QSEN into
Hospital Practices
Deb Tauber, MSN, BSN, CEN
Stephanie Teets, MSN, BSN CNL
Katherine Weibel, BSN, MBA, RN-BC
Chamberlain College of Nursing
Adventist Midwest Health
CONFIDENTIAL ©2014 Chamberlain College of Nursing, LLC. All rights reserved. 0713ccn
Disclosure Statement
Deb Tauber, Stephanie Teets and Katherine Weibel
have no financial or commercial interest in this content.
Objectives
Learner will be able to describe the process of using this
methodology to integrate QSEN into the hospital setting,
by incorporating QSEN into the hospital orientation process.
Demonstrate how teams of healthcare professionals
can integrate the competencies of the QSEN process
into “Rapid Response Mock Training.”
Participant will be able to compare this opportunity to
current needs in their organization or nursing school
and construct a similar opportunity to meet their
specific challenges.
Call From Above
Adventist Hospital Leaders recognized QSEN as
a potential opportunity for improving patient safety.
The first principle for designing safe systems in health care organizations is –
according to the IOM report To Err is Human — to provide leadership from
the top-most level of the organization. The need to create a safe and effective
nursing environment clearly parallels, and indeed overlaps, this IOM dictum.
(The Joint Commission, 2012)
What Exactly is a Competency?
The IOM defined competency as “the habitual and
judicious use of communication, knowledge, technical
skills, clinical reasoning, emotions, values and reflection
in daily practice” (Brady, 2011).
5
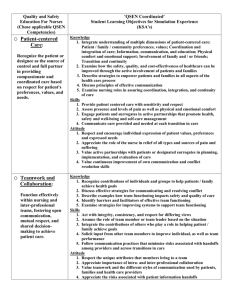
Quality and Safety Education for Nurse (QSEN)
• QSEN Competency Categories
• Quality Improvement
• Patient Centered Care
• Safety
• Teamwork and Collaboration
• Informatics
• Evidence-Based Practice
The purpose of the QSEN competencies is to meet the challenge of
preparing nurses to improve the knowledge, skills and attitudes (KSA’s)
necessary to continuously improve the quality and safety of healthcare
systems within which they work (Adapted from QSEN, 2009).
6
Evidence Based Practice (EBP)
• Implement each competency with evidence
• Gather best practices
• Review current healthcare education, nursing and
patient safety literature
7
Addressing Disruptive Behaviors Incivility
in Healthcare
A summary of relevant sources of literature support the findings
that the problems of incivility in healthcare are both harmful and costly.
Replacement of one nurse can cost an organization between
$46,932 - $145,000 (Kennedy, Michols, Halamek, & Arafeh, 2012).
“Workplace incivility may be subtle but it creates a heavy financial
burden estimated at $24 billion dollars annually” (Spence, Laschinger,
Cummings, Wong, & Grau,2014).
8
Summary Graph Data (Tauber, 2014)
9
Safety
It is well documented in many initiatives leading healthcare
organizations driving improved outcomes (AACN), World
Health Organization (WHO), QSEN, The Joint Commission,
that the benefit of Interprofessionality will improve patient
outcomes and decrease sentinel events.
10
What is Simulation?
“A technique, not a technology, to replace or
amplify real experiences with guided experiences,
often immersive in nature, that evoke or replicate
substantial aspects of the real world in a fully
interactive fashion” (Gaba, 2004,p 2).
Gaba, D. (2004) The future vision of simulation in health care. Quality
and Safety in Health Care, 13 (Suppl 1), 2-10.
11
The Value of Simulation
• Safe environment
• Learn from mistakes
• Repetition
• Enhance teamwork and collaboration
• Improve
-
Critical Thinking
Judgment
Organization
Prioritization
Communication
• Controlled environment
12
Mock Codes
• Mock rapid response
• Mock code blues
• Mock stroke alerts
• Debriefing afterward
• Mock cardiac alerts
13
Three Phases of Debriefing
(Harvard Model - CMS)
• Reactions - Clear the air and set the stage for discussion
- Feelings (normalize)
- Facts
• Understanding
- Exploring - explore trainees perspectives on scenario events
- Discussion and teaching
• Summary - distill lessons learned for future use
- What worked well
- What should be changed next time
- Major take always
14
Evaluation Tools
15
Integrating QSEN into Clinical Practice
Socializing QSEN
• Introduction to the CNOs with commitment
• Presentation to nursing leadership, education team,
Advanced Practice Nurses
• Discussions at Patient Care Division Meetings
• Introduction at orientation
16
Integrating QSEN
Revised curriculum for the New Grad Residency Program
integrating QSEN competencies into each cohort meeting.
17
Example Curriculum
18
19
20
As a Beta testing group –
we piloted the use of this
onboarding checklist with
16 New Graduate Nurses
and their preceptors.
21
Feedback from Beta Testing Group
• Overall the feedback from the group has been very positive.
We are using process improvement for evaluating and
improving for the next groups. One of the gaps identified
has been getting the behavior portion documented for fear
of possible consequences. We hope to improve this.
• The hope is as the "culture" within the organization
changes and people become more comfortable with
behavioral expectations it will be easier to hold people
accountable for their behavior.
22
Next Steps
• We will evaluate the orientation model and modify
as needed from our BETA testing group
• We intend to submit this information for publication
• Compare HCAPHS, Press Ganey, Core Measures in one
specific unit for one year and see if any measurable
differences are noted
23
References
Gaba, D. (2004) The future vision of simulation in health care. Quality
and Safety in Health Care, 13 (Suppl 1), 2-10.
INACSL,(2011). Standards of Best Practice: Simulation. Clinical
Simulation in Nursing, 7(4), S3-S7.
Fero, L., Wesmiller, S., Witsberger, C., Zullo, T., Hoffman, L., Critical
Thinking Ability of New Graduate and Experienced Nurses, Journal of
Advanced Nursing, 65(1). 139-148.
Brady, D. S. (2011). Using Quality and Safety Education for Nurses
(QSEN) as a Pedagogical Structure for Course Redesign and Content.
International Journal Of Nursing Education Scholarship, 8(1), 1-18.
doi:10.2202/1548-923X.2147
24
References Continued
Spence Laschinger, H. K., Cummings, G. G., Wong, C. A., & Grau, A. L.
(2014). Resonant Leadership and Workplace Empowerment: The Value
of Positive Organizational Cultures in Reducing Workplace Incivility.
Nursing Economics, 32 5-11.
Tauber, D. A. (2014). [Simulation respectful caring assertive
communication evaluation tool]. Unpublished raw data
25