Graham Rutt - Northern Deanery
advertisement

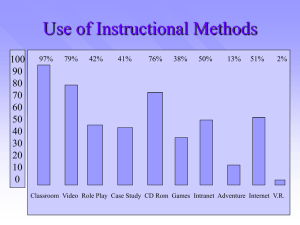
Welcome to Health Education North East Postgraduate School of Primary Care Graham Rutt Director June 2014 Introduction to all the less exciting stuff But it’s important nevertheless… Graham Rutt, Director Postgraduate School of Primary Care Nb: the links in this ppt. only work if you view it as a slide show… Who does what? • Health Education England – Delivery of all aspects of education and training • RCGP – Setting standards, curriculum and exams • GMC – Regulation of doctors and educational systems • NHS Employers – Terms and conditions of service for trainees • Health Education North East – Local LETB and part of HEE • Medical and Dental Advisory Group – Responsible for overseeing the organisation of what we do • The Dean – Accountable to the GMC for the training, assessment and revalidation of all trainees • Postgraduate School of Primary Care – Us!! PGSPC 2014 Director School Board Head of Continuing Practice Associate Directors for Continuing Practice (Remediation, Returners) Advisors for Continuing Practice Lead Training Programme Directors (Appraisal + Revalidation, Sessional GPs) (Rotations, Trainee remediation, Trainer training, Curriculum Planning) Associate Directors for Specialty Training (R+S, ARCP, QM, Faculty Development) Training Programme Directors GP Tutors (Taught Course delivery, QC of posts, Trainer support and apparaisal, Trainee support, exam preparation, IMG support) (QA Appraisal, Education, Remediation) (half-funded by LAT) Hospital Clinical Supervisors 172 (head count) Out of Hours Clinical Supervisors GP Educational Supervisors 283 (head count) The context • • • • • • 3 million patients 2342 GPs (2125 wte) 523 Trainees Best place in the world Most rural county in England (Northumbria) N.b. • The School contracts with trainers to provide a service • You employ the trainees • We are all in this together • If you are ever concerned about a trainee phone your TPD and read the advice about managing concerns: information-for-trainersand-tpds/managing-trainees-in-difficulty Overriding philosophy • Caring and compassion; common sense and problemsolving are core skills for GPs • Caring for the practitioner and learner-centredness are core skills for trainers of GPs • It is more important to teach problem-solving skills than the solution to each problem (just as with patients) – Thus the skills focus to the ITC so that new trainers can teach about anything, not just about specific subjects. – Hence the focus on flexibility, adaptability and learner centredness Philosophy of teaching • Becoming a good GP will help you pass your exams, not vice versa – Thus the resistance to the pressures to focus on exam technique in GP training • Training should involve signposting to other resources when knowledge alone is needed – Thereby freeing teaching time to reflect on real-life experiences. • There is no single right way to teach or learn, but there are many wrong ways – E.g. if viewing the consultation using one model is not help, try another… Questions so far? The RCGP GP curriculum • Written by the RCGP • Approved and signed off by GMC • Sets out what is required to practice as an independent General Practitioner in the UK NHS. • Defines the knowledge, skills and qualities expected of GPs • Describes useful learning and teaching activities. Curriculum contd. • Forms the foundation for GP training and assessment across the UK • Download the Introduction and user guide • Do this tonight (well next week anyway) • Explore any areas that interest you • No need to remember it all – the e-Portfolio does that for you MRCGP • Integrated assessment system, • Must be passed before trainees can apply for a certificate of completion of training (CCT) and full Membership of the RCGP. • Comprises three separate components: – Applied Knowledge Test (AKT) – Clinical Skills Assessment (CSA) – Workplace Based Assessment (WPBA) MRCGP contd. • Tripos • Each test different competences using validated assessment methods • Together cover the spectrum of knowledge, skills, behaviours and attitudes defined by the GP Specialty Training curriculum. AKT • Summative assessment of the knowledge base that underpins independent general practice • Trainees who pass will have demonstrated their competence in applying knowledge at a level which is sufficiently high for independent practice. • For those who like to know more: MRCGP FAQs [PDF] CSA • Summative assessment of a doctor’s ability to integrate and apply clinical, professional, communication and practical skills appropriate for general practice. • Simulates a typical NHS surgery clinic with a range of scenarios from general practice relevant to most parts of the curriculum which can also target particular aspects of clinical care and expertise. • For those who like to know more: MRCGP FAQs [PDF] Commonest reasons for failing? • Many described • Overiding themes: – – – – Poor exam technique Over-thinking Forgetting what the A stands for (Applied…) Concentrating on own performance and not what the simulator has just said (the simulators are paid to deliver the relevant cues: listen and thou shalt pass) – Not being good enough Help? • Loads available via Training Programmes for trainees struggling to pass these exams • Frequent topic at educator conference, trainer plenaries and trainer groups for trainers wanting to learn some strategies to help their registrars Workplace Based Assessment (WPBA) • Evaluates the trainee’s progress in areas of professional practice best tested in the workplace • Provides an opportunity for gathering evidence and reflecting on performance • Evaluates aspects of professional behaviour that are difficult to assess in traditional examinations • Provides constructive feedback on areas of strength and developmental needs, identifying trainees who may be in difficulty • Drives learning in important areas of competence WPBA contd. • Determines fitness to progress to the next stage of training • Includes formal tests and reflection on naturally occurring evidence (“Learning Logs”) Is the trainee’s responsibility to organise, undertake, collect, log etc etc, NOT the trainer’s Commonest reasons for failing? • Many described • Overiding themes: – Poor reflection – Not enough evidence – Not being good enough Note that it is not a numbers game – 1 high quality entry is better than 10 poor quality one, and the assessment process acknowledges that What is “reflection”? • Important guidance on reflection available at: http://www.northerndeanery.nhs.uk/Northern Deanery/primary-care/gp-specialisttraining/ReflectivewritingguideHENE.pdf Help, show me how to do one…. • No!! • Why not? – Full guidance on the use of all the tools is available at: • • • • • • • • Case-based Discussion (CbD) Consultation Observation Tool (COT) for use in primary care only Multi-Source Feedback (MSF) Patient Satisfaction Questionnaire (PSQ) for use in primary care only Direct Observation of Procedural Skills (DOPS) Clinical Evaluation Exercise (MiniCEX) for use in hospital posts only Clinical Supervisors Report (CSR) to be undertaken in all hospital posts, but can also be used in the primary care setting Learning Log and Personal Development Plan (PDP) And… • Guidance notes are available on the e-Portfolio every time you do one • The basic principles of feedback-giving remain exactly the same, whichever tool you use • You will forget everything I say between now and go-live or the effort needed to remember everything will drive out the other more important lessons you have been studying • I want you and your trainees to enjoy the rest of your lives And… • No single piece of evidence is quite as important as we think it is (By the time they finish, the average trainee has amassed 800 pages on their e-Portfolio. If you haven’t quite got one of them right, so what?) • You will get many more chances to explore the specifics during your Supervisory training • There are always friends you can phone within the school. Someone somewhere is always available to listen…. • Frequent topic at educator conference, trainer plenaries and trainer groups for trainers wanting to learn some strategies to help their registrars Clinical supervision • Relates to trainees working in your practice • Its what the tutors have been teaching you to do • Make sure assessments do not get in the way of teaching • When writing the report, be honest etc • Excellent guide for starters available at: Writing clinical supervisors reports e-learning module Educational Supervision • GP Trainees have the same ES throughout training • Normally work in your practice at some stage • Meet at start of training and then twice a year to review progress (the ESR) • Be available for advice • Regularly read and comment on the trainee’s log entries • Not expected to be the resource for extra support if struggling: TPDs do that Purpose • Ensure regular feedback and engagement with the ePortfolio • Provide a report for the official Annual Review of Competence Progression (ARCP) process • Every year an ARCP panel examines if the trainee is making satisfactory progress, and if not what needs to be done • The panel needs a recent ESR to inform their decision making. • Note that the panel makes the decision, not the ES • Review meetings usually take between one and two hours, followed by a write-up in the ePortfolio. Educational Supervisors Review • Excellent guide available at: Educational supervisor review – a step by step quick reference guide [PDF] • Comment on the evidence in the e-Portfolio relating to 12 Competence Areas • If ever formulating the opinion that unsatisfactory progress is being made or if ever unsure whether to "grade" as satisfactory/ unsatisfactory or panel opinion requested - phone your TPD and ask for support and advice and read the advice about managing concerns: information-for-trainers-and-tpds/managingtrainees-in-difficulty Key issues • Quality of evidence is more important than quantity. • In the early stages of training, the evidence will be patchy • The review should form the basis of a learning plan, highlighting where a trainee is doing well and where more support is needed. • By the end of ST3, the educational supervisor will be looking to establish fitness to practise through several sets of evidence in each competence area, collected from a range of settings and through different tools. Each portfolio will look slightly different, but it should provide a rich picture built up over three years. It’s still the panel that makes the final decision, not the ES What happens at panel? • Recommendation of unsatisfactory progress should not be a surprise at panel. • At an ARCP panel, e-Portfolios are looked at in detail by at least four trained panel members, including lay and external representation – a) at the end of ST3 – b) if there is a concern – c) 10% of all the rest Useful links • RCGP Trainee ePortfolio • Information for trainers, supervisors and deaneries • ESR-step-by-step-Guide-November-2013v4_2 • information-for-trainers-andtpds/managing-trainees-in-difficulty Useful texts The Essential Handbook for GP Training and Education Ramesh Mehay The Inner Apprentice Roger Neighbour