Doctors in Difficulty Workshop
Medical Educators Conference
7
th
Nov 2014
Doctors in Difficulty Workshop
Dr Mumtaz Patel
Consultant Nephrologist
Divisional Educational Lead
Manchester Royal Infirmary
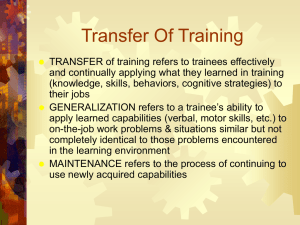
Doctors in Difficulty Workshop
• Outline and Aims
• Definition
• Categories of Difficulty
• Common Presentations
• Potential Triggers of Doctors in Difficulty
• Managing Doctors in Difficulty
• Case Studies
Definition:
“Any trainee who has caused concern to his/her educational supervisor(s) about the ability to carry out their duties, which has required unusual measures.
This would mean anything outside the normal trainertrainee processes where the Training Programme
Director has been called upon to take or recommend action.”
(NW Deanery, 2013)
Categories of Difficulty
Trainees in Difficulty
Struggling to manage workload, failure to progress
Trainees with Difficulties
Illness, Home or personal life issues
Difficult Trainees
Inappropriate, unprofessional behaviours. Lack of
Insight
Categories of Difficulty
Performance Issue
Problematic Personal Conduct
Problematic Professional Conduct
Health problems
Learning Environment
System Issues
Common Presentations
Work Based
• Absenteism/lateness
• Poor time management
Clinical Performance
Cognitive
•
Over/under investigating ;missed diagnosis
• Failure to follow guidelines/policies
• Complaints; incidents
• Memory problems, Poor problem solving/decision making
• Poor concentration, attention, learning problems
Language/Cultural
Psycological/Personality
• Poor verbal fluency
• Poor understanding
• Irritable, forgetful, arrogance, lack of insight, denial
• Highly self critical; perfectionist
Social
• Isolation, withdrawal, irritability
• Poor interpersonal skills; lack of insight
Potential triggers of concern
Patterns or repetitive behaviours (rather than one off
Sudden out of character behaviour
Sickness
Serious one-offs that are rationalised by trainee
Eg. a small lie
Early Signs and Identification
Steps in Management
1. Early Identification of problems and intervention is essential.
2. Establish and clarify the circumstances and facts as soon as possible – Access many different sources of information.
3. Remember poor performance is a symptom and not diagnosis and needs to be explored.
4. A robust and detailed diagnosis can lead to effective remediation.
5. Clear documentation is essential.
6. Misgivings must be communicated; Records must be kept and remedies must be sought
Managing trainees in Difficulty
• Trigger Event or Incident
Is it important?
Does it matter?
Who do I need to involve?
• Consider CS, ES, TPD,
DME, Deanery, HR, OH
Investigate
• Investigate and define problem
• Collate evidence, DOCUMENT.
Be objective
Think patient and person safety at all times
• Be objective
• Do n0t jump to conclusions
• Formulate opinion
Decide
• Individual issue
• Organisational issue ?both
System failures easy to overlook
• Be fair and objective
Taken from NACT Managing Trainees in Difficulty 2012
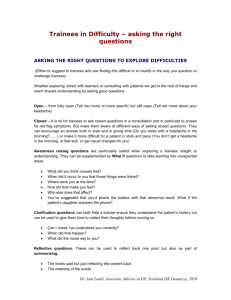
Three Questions
Does it matter?
Can they normally do it?
Why are they not doing it now?
• If no, relax
• If yes, do something and ask
• If no, re-trainable?
• Not trainable, exclusion only!
• If yes, ask
• Clinical performance
• Personality issue
• Health
• Learning Environment
Key areas to explore when considering poor performance ie.
‘Potential Diagnoses’ i) clinical performance ii) personal, personality and behavioural issues including impact of cultural and religious background iii) physical and mental health issues iv) environmental issues including systems or process factors, organisational issues including lack of resources
Taken from NACT Managing Trainees in Difficulty 2012
Levels of Concern - 1
No harm/risk to patient, staff, trainee.
Minor incidents, complaints
Controlled illness
Failure to attain training goals
Action plan ES lead, thorough documentation.
Discussion with trainee/minor investigation
Pastoral Support/OH
SMART action plan/short resolution time.
Discussion with TPD/?HR, Lead Employer
Levels of Concern -2
Potential or actual harm/risk to patient, staff, trainee or reputations.
Repetitive patterns, recurrent behaviours
Any issue requiring extension of training
Action plan
Formal Investigation
HR, OH, Deanery, PGME
Action plan with defined objectives
Specialised interventions
Levels of Concern - 3
Actual serious harm, reputations are at serious risk
SUIs, Formal complaints
Criminal Act
GMC, NCAS referral
Action
HR, OH, Deanery, PGME
As level 2 with formal investigation
? Cessation/Restriction of practice
Managing Clinical Concerns
Specific areas, technical and non-technical skills
Focused retraining
Often task orientated and with specific targets
Performing adequately at a level (eg ST 3) but not demonstrating the necessary skills eg leadership, complex decision making to progress to a higher level.
Focused training
Mentoring and Coaching
Thorough documentation
Managing Personality Issues
Close clinical supervision, developmental mentoring
Develop insight
Cultural and Religious advice if necessary
Simulation or videoing to challenge behaviours
Educational Psychology
Cognitive Behavioural Therapy
Difficult and sometimes impossible to remedy
Managing Health Issues
Doctors can become ill
Physical and mental Illness
Substance misuse
Occupational health review
Disability act requires employers to make reasonable adjustments
Ensure adequate support
Staff counselling
Causes of Management Failure
Early concerns not addressed
Inadequate documentation of problems and discussions; dated and signed
Insufficient thought given to remedial plan
Feedback especially around ARCP outcome 2 and 3 is seen as arbitrary and punitive
Views on course of action are varied
Important Messages
Further important messages
General points
Document everything
Be transparent
Discuss actions and plans with trainee
Support
Staff counselling
Share appropriately
PGME, Deanery.
Managing Trainees in Difficulty
Managing Trainees in Difficulty
Managing Trainees in
Difficulty
(version 2)
Practical Advice for Educational and Clinical Supervisors
July 2012
NACT UK: Supporting
Excellence in Medical
Education
PGD Structure
Associate Medical
Director (eduction)
PGD structure
DME
Associate Director
Med Ed
Head of
Postgraduate
Education aDME aDME aDME
Ed Sup
Div Lead
Clin Sup Junior Rep
Developing DiD support within
CMFT
Website
Blog
Interactive toolkit
Links to useful documents and sites
Intelligence
Referral to PGME of DiDs
Involvement of ES in sickness management
Trainer involvement
Faculty of mentors
Assessment and targeted training groups
Education
Trainer development days