Orkney Health & Care presentation
advertisement
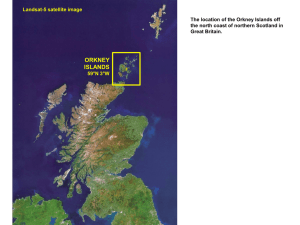
Orkney Health and Care Working together to make a real difference 28 March 2014 Judy Sinclair, Lead Nurse Lynda Bradford, Service Manager, Health and Community Care Aims of Workshop: Explore how RGSW may support service improvement within the context and challenges of integrated care delivery in Orkney Using the NES Skills Maximisation Toolkit: 1. Clarifying the patient journey 2. Capturing uniqueness 3. Creating improvement 1. Clarifying the patient journey- what’s happening now? Steps and activities involved when service user beginning the journey How do service users and carers/ families access the service 2. Capturing uniqueness-what’s the best contribution? Who currently undertakes the various tasks and activities What tasks need the skills only a registered practitioner can provide What could be done by the RGSW Identify any other issues 3. Creating improvement- making it happen • Focus on what the RGSW could do • Suggest changes to positively impact on patient journey • Suggest positive changes for the team and team working • Improving the service by using the RGSW • Contribute to the way forward 20 Participants from a range of backgrounds: ◦ Service managers, community nurses, physiotherapists, occupational therapists, intermediate care team nurses and rehabilitation support workers, social workers, home care, practice education for nursing and allied health professions and Orkney College Lecturer. An interactive workshop Background information had been sent in advance for consideration of a patient journey Ways of working were agreed by the group: ◦ ◦ ◦ ◦ ◦ Focus on the RGSW role Give up some existing beliefs Think differently and out with comfort zone Implications of not changing The Car Park Commonalities across teams and geographical areas i.e lack of services in isles, identifying need but can’t meet them, remoteness, expectations of clients, families and communities, multi assessments Differences across teams and geographical areas i.e service capabilities and capacities, inconsistencies in health and social care roles, differing professional cultures, communication – with who, by who Gaps in service provision: i.e. Continuity of some AHP programmes, respite care, limited 3rd sector in some areas, different crisis response, different overnight provision, facilities and equipment Who currently carries out which activities and why? Could any of these activities be carried out by a RGSW? What other tasks/activities could be carried out by the RGSW? What could be carried out by RGSW: Pre-discharge Referral and outcome focussed assessment Home preparation Working with OT, physio and nursing staff Preparation of furniture/bed Discharge Support getting home – travel can be difficult/air/sea Continuation of programmes of care OT and personal care links Accessing equipment Agreeing outcomes with client/family At Home A range of activities in conjunction with OT, Physio, Home care and nursing such as: Personal care, meal prep, exercises, nutritional needs, support with medication, continence assessments, use of telecare, telehealth etc Rehabilitation in the home environment Facilitate social engagement Liaison with multi-disciplinary team Groups were asked to consider the potential RGSW role in Orkney: What are the opportunities and benefits? What are the challenges of introducing the role How would you overcome these challenges? What knowledge/skills will be required to deliver the desired service/outcome for clients Island sustainability Ability to be person centred Earlier discharge with attendant benefits Reduced hospital admission Safer discharge and reduced readmission Service users able to stay on island Career development/ improvement for registered staff Continuity of care Delivery of service user vision Cultural shift required Boundaries of role and knowing limitations Existing terms and conditions of employees Potential lack of confidence by professionals, clients and public Potential for duplication Supervision and mentorship Developing and maintaining clinical currency and governance Funding Expectations of professionals, clients and public Magic wand! Clear criteria - clarity about what is ‘Needs’ and what is ‘Wants’ Minimum training and standards - Education programme that is available, reasonable, local, using a blended approach Flexibility in system of workers Harnessing IT solutions Integrated and shared clinical communication Regular supervision and support Contract issues Isles network of care – VC network and connectivity issues Isles differences Gender issues Capacity Transport – ferry/air Risk management 24/7 cover Organisation of workload Who owns it – health or social care? Continuity of care, enabling people to be at home Better outcomes for clients and their families Improved patient centeredness for complex LTC conditions Based on the island and flexible Improved, earlier discharge and rehab at home Skills and knowledge for rural and island areas Maintain island life, create opportunities Better linkages with other services Something I’ve learned from today; All parties on board – the tide has turned, it can be done Other services’ challenges Gaps in service Professional roles and responsibilities Value of education – essential starting point How inflexible some professionals are The importance of multi disciplinary discussion Clarification of the RGSW role What did you enjoy most about the day? Meeting other folk and getting the bigger picture Networking Person centred approach Well structured programme and ideal group sizes Exchanging and challenging ideas with others Good discussion about the RGSW role What could have been better? A service user point of view (5) Couldn’t have been better More folk from the isles (2) Could have discussed the intermediate care team more to discuss existing roles and comparisons Orkney Health and Care Working together to make a real difference Questions?