Urgent-Care-Presentation-LEB-11-July-13
advertisement

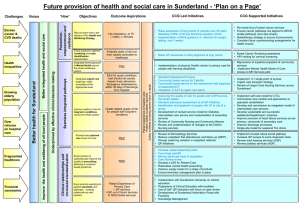
Urgent Care Planning in South Tyneside David Hambleton Urgent Care Everyone’s problem Urgent Care Plans • Urgent Care – – Everyone’s problem so nobody’s problem • Why is it a problem – High A&E attendances but – Low admission rates – Lots of people in A&E who needn’t be Percentage of A&E Attendances converting to Admissions 3 Over-crowding in A&E Why it’s a very bad thing • After admission through a crowded A&E 43% increased chance of dying at 10 days • A&E stay of 4-8 hours increases inpatient length of stay by 1.3 days • A&E stay >12 hours increases inpatient length of stay by 2.35 days What can be done prior to A&E • GP Access • Quality Premium (GP QOF) – Ambulatory Care Conditions – A&E usage • • • • Anticipating urgent care demand Improved care in nursing homes STICS - better management of LTC RAID - rapid, effective and safe access to mental health services What can be done in hospital • • • • Ambulatory Care Conditions pathway GP in A&E? White board system to track patients Review spilt of beds between medical and surgical specialties • Rapid response clinics • Psychological liaison service within an Urgent Care hub Discharge & out of hospital care • Hospital discharge process and communication • ‘Time to think’ beds • Single point of contact for social care • Reviewing current provision of self management education and support NHS 111 update • • • • • • National free-to-call memorable number Single point of contact for urgent care ‘Talk before you walk’ NE system is working (unlike others) Teething problem being ironed out Opportunities still to be realised NHS 111 update • Patients directed to right services, first time • Directly booking appointments into services – including GPs • Better use of community services • Indentify where gaps in service are Teams involved Programme for implement DRAFT URGENT CARE SYSTEM MAP – South Tyneside Urgent Care Delivery Group Self Care Supporting older people at home • STICS (COPD) • STICS (COPD) • Nursing home SLA/ LES • Community matron as care coordinator (evaluation) Crisis • ACS Pathway review • Single point of contact social care Acute setting Step down • IRT • Time To Think beds • Discharge process • Discharge Communication •Dementia Step up facilities •Perth Green • PPP patients • Telehealth/ wound sense Supporting older people at home • STICS (COPD) • Nursing Home SLA/ Spec Self Care • Pulmonary Rehab • Cardiac rehab •Pulmonary Rehab •Cardiac Rehab • DNs/ flu vaccines • Zoning of Urgent Care nursing teams *Primary care *Primary Care *Community nurses (map which teams) Shared Care Plans *A&E *Local Authority *Community nurses (map teams) * Hospital staff * SW team * LA * FT *Primary Care *Community Nurses (map which teams) *Rehab teams Tools Risk stratification - (in use in a fragmented way, i.e. separately in FT and Primary Care); not yet in use in LA = opportunity to streamline, agree consistent cohort? e.g. at risk of admission Standard Care Plan – opportunity Standard work – across the pathway for this group involving teams and shared understanding, + time based standards = opportunity (see Nottinghamshire work in progress on frail elderly pathway care standards) Round Table Discussion • On your tables you will be asked to consider: • Are we on the right lines with our plans? • What else should we be thinking about doing?