Hospital autonomy: Vietnam experiences
IMPLEMENTATION OF HOSPITAL
AUTONOMY: VIETNAM EXPERIENCES
Health Strategy and Policy Institute - Vietnam
Content of presentation
1) Introduction of public hospital network
2) Introduction of policy on hospital autonomy VN and
Implementation
3) Experience of Vietnam from an evaluation of hospital autonomy
Hospital network in Vietnam
Public Private
(137813 beds ) (> 7000 beds )
Advance care
Essential care
Basic care
40
Hospit als
235 Provincial
Hospitals
705 District Hospitals
(including 48 Hosp. of other sectors) +
607 regional policlinics)
10,979 Commune Health Stations
>95 private hosp., (04 foreign-funded hosp.)
Private practitioners
Hospital autonomy policy
(Cont.)
Objectives of Decree 43/2006
1) Better health services delivery, improve quality and increase hospital revenues
2) Social mobilization of resources for health sectors in order to reduce subsidy from government to health facilities
Experience of Vietnam from an evaluation of hospital autonomy
The evaluation conducted by HSPI and number of departments of MOH
Time: Oct to Nov 2009 (after 3 years of policy implementation)
Side of study: 18 hospitals included:
7 central hospital (2 fully autonomy)
5 provincial hospitals (1 fully autonomy)
6 district hospital
Objectives of evaluation
1) To analyze the implementation process of Decree No. 43 in hospitals and to review the organization of implementation based on the legal documents concerned.
2) To assess the results from implementing Decree No. 43 in public hospitals in terms of task accomplishment, organizational structure, staffing and financing.
3) To make recommendations as related to the current autonomy policy to assure efficient, equity and development oriented supply of health services.
MAIN FINDINGS
Positive impacts of hospital autonomy (compare 2008 to 2005)
Organization: Hospitals are more active in rearranging their departments and wards and human resource as well
Technical activities:
More active in expanding types of healthcare services that help increase the number of patient contacts to hospitals (outpatient:1.3
– 1.5 times, in patient: 1.2-1.4 times)
BOR increased 13 - 25%
Average number of lab tests/patient contact has increased by 1.3
- 2.1 times.
The average number of CT-scanner tests/patient contacts increased by 2-3 times at provincial and central hospitals. The average number of ultrasound tests/patient contact increased by
1.4 - 1.5 times.
MAIN FINDINGS
Positive impacts of hospital autonomy:
In terms of finance:
Hospital revenues increased by 1.8 times - 3 times (the main increase found from the technical services )
Expenditure for health services increased 2-2.8 times
Change in hospital expenditure: spending for HRH increased
1.8 -2.7 times;
Hospital staff’s income increases increased 0.5 – 2.3 times
Investment in medical equipment are increased .
MAIN FINDINGS
Hospital autonomy may lead to the following threats
Service abuse to make profit by:
- Increasing unnecessary hospital admission for inpatient care to increase hospital revenues.
- Lengthening hospitalization stay (central hospitals: 9.4 days up to
10.1 days; provincial hospitals: 6.8 days up to 7.4 days; district hospitals: 5.8 days up to 6 days)
Service abuse to make profit by:
- Tendency of increasing utilization of high tech laboratory tests and equipment to increase the revenues
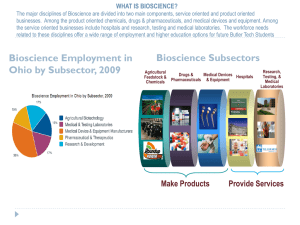
Use of CT & MRI in central hospitals
CT
Bạch Mai
2005 2006 2007 2008
0.024 0.031 0.042 0.045
K TW 0.057 0.082 0.105 0.148
BV Bình Định 0.013 0.014 0.021 0.056
Bv Chợ Rẫy 0.065 0.066 0.070 0.072
ĐK TW Huế 0.028 0.029 0.035 0.036
Mắt TW 0.006 0.007 0.007 0.006
Hình 1. Số lần chụp MRI/lượt BN qua các năm Bảng 20. Tỷ lệ sử dụng CT/lượt BN qua các năm
Tỷ lệ tăng
2008 so với 2005
1.8
2.6
4.4
1.1
1.3
1.0
- Binh Dinh hospital: CT use/patient increased by 4.4 times
- 20% of doctors in the staff survey responded there would be lab-test overuse.
MAIN FINDINGS
Hospital autonomy may lead to the following threats
Affected service quality
- hospital of overcrowd (BOR 103% - 172%),
- heavy workload in almost all hospitals while lack of staff
(nurses/doctor low with 1.9 nurses/doctor compare to requirement as
3 – 3.5)
Average expenditure per one treatment
Treatment cost increase (in 2008 compare to 2005)
Bệnh viện
Hospital
Chênh lệch chi phí BQ 1 lượt khám bệnh (2008 và 2005)
1.82
1.29
2.97
2.25
Chênh lệch chi phí BQ 1 đợt điều trị nội trú (2008 và 2005)
1.58
2.10
1.83
2.24
The expenditure for medicines occupied 56% to 65% total expenditure for technical services
MAIN FINDINGS
Hospital autonomy may lead to the following threats
The gap in terms of benefits among hospitals at different levels in autonomy implementation: hospital autonomy brings more benefits for central hospitals, due to
+ higher revenue
+ higher income for health staff
+ easier for investment
Create a bigger gap in attracting and retaining health workforce to work in rural areas
What government need to consider
The diversification of private investment in public hospital without strong regulation create the tendency of privatizing the public hosp toward f orprofit
Join venture/sharing benefit
Priv a te /M ark et
Self operation budget
Op ein g Pu b lic
Basi c Publ i c
Private/Public
Mix
B- Budgetary units
A- Autonomous units
C- Corporatized units
P- Privatized units
B A C P
2002 2008
What government need to consider?
Policy warning:
High risk of “selective services” with investment is mainly for hightech equipments and easy to collect the revenues.
Risk of service overuse or abuse lead to increase the expenditure for health and OOP as well as patient safety.
Weak hospital performance regulation and management
• Financial transparence
• High-tech services investment
• Quality control
• HMIS
What further evidences are needed?
- Impact of hospital autonomy to service quality, patient safety, equity
- Health technology assessment for more effective investment and rational use of technology