Uploaded by
Mindzie Metayer
Sexually Transmitted Infections: Nursing Management & Prevention
advertisement

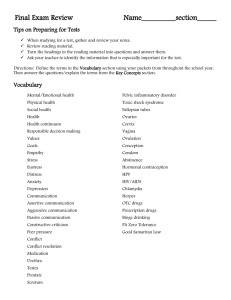
NUR3219C Sexually Transmitted Infections Learning Objectives • Identify factors contributing to sexually transmitted infections (STIs). • Describe the etiology, clinical manifestations, complications, diagnostic studies, and interprofessional care for chlamydial infections, gonococcal infections, trichomoniasis, genital herpes (HSV), genital warts (HPV), and syphilis. • Distinguish between primary, secondary, and tertiary syphilis. • Describe the assessment, interprofessional care, and nursing management of women with pelvic inflammatory disease (PID). • Prioritize nursing interventions for managing acute STIs. • Summarize the nursing role in the prevention and control of STIs. 2 Overview: Sexually Transmitted Infections (STIs) • Infectious diseases spread through sexual contact with the penis, vagina, anus, mouth, or sexual fluids of an infected person • Easily treated but still a serious health threat due to potential complications which include infertility and cancer • Affects well-being, relationships, and sex life • Nursing roles: education, counseling, and referral 3 Sexually Transmitte d Infections • Bacterial infections • Chlamydia • Gonorrhea • Syphilis • Parasitic/protozoan infections • Trichomoniasis •Viruses • Genital herpes • HIV • Hepatitis B and C • HPV • Molluscum 4 Transmission • STIs can also be spread • Skin-to-skin (HPV) • Via blood or blood products (HIV or mother to baby) • Autoinoculation (spread through touch of infection) • Not typically transmitted from inanimate objects or casual contact 5 Background • Rates of STIs are at an all-time high • Nearly 26 million (1 in 5 adults) new infections occur in the United States each year; $16 billion in health care costs • All sexually-active persons are at risk • Contributing to increased risk are socioeconomic factors, decreased condom use, cuts to STD programs across the country 6 Reporting • In the United States, all cases of gonorrhea, syphilis, and chlamydia must be reported to public health authorities for surveillance and partner notification • Attempt to prevent and control the spread • Only a small percent of new STIs are reported • 2 million cases reported annually; does not represent actual number of infections 7 Risk Factors for STIs • High-risk behaviors • High-risk medical history • Trends in contraception • High-risk populations 8 Nursing Management: STIs Assessment • Subjective data • Sexual health history • Sexual activity with individuals with STIs • Past history of STIs • Multiple sexual partners • Unsafe sexual practices • Medications: allergy to antibiotics • Functional health patterns • Objective data • General • Integumentary • GI • Urinary • Reproductive • Diagnostic findings 9 Nursing Management: STIs Assessment • Awareness topics for HCPs • Gender identity, current anatomy • Risk history and sexual behaviors • Number of partners in last month? Year? • Types of partners; men, women, both? • Type of birth control; condoms, barrier methods • History of STI • Drug/alcohol use • Exchange of sex or drugs or money • Risk for violence and personal safety 10 Nursing Management: STIs Assessment • Interpersonal skills • Respect • Compassion • Nonjudgmental attitude • Tailor counseling to individual • Do not assume: • Heterosexual, MSM, WSW, or same sexual practices due to appearance • Older people are not at risk • Psychologic support • Emotional responses include embarrassment, shame, guilt, anger, vengeance • Provide counseling and support 11 Implementation • Health promotion • Discuss safer sex and harm reduction • Sexual abstinence is the only certain method of avoiding all STIs • Established, monogamous relationships have lower risk of STIs • Address issues related to drug and alcohol dependence • Address issues of special populations • Encourage HPV vaccination • Give parents accurate and current information to decrease fears • Reinforce cancer prevention • Screening programs • Effective for identifying, treating, preventing transmission and controlling the spread of STIs 12 Implementation • Measures to prevent infection • Proper condom use • Refusal of sex without condom is safe and legitimate • Educate on the availability of HIV PreExposure Prophylaxis (PrEP) and postexposure prophylaxis (PEP) • Help patients be aware of specific signs and symptoms of infection of themselves and their partners • Remind that most STIs may have no symptoms 13 Questions? Please post to the discussion board in Canvas or reach out to your course instructor!