Uploaded by
Elisa Mchunguzi
Human Embryology: Gametogenesis, Spermatogenesis & Oogenesis
advertisement

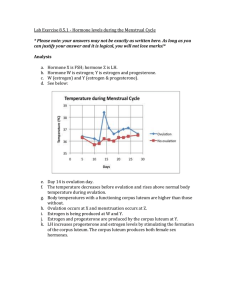
Human Embryology GAMETOGENESIS Dr. Ali K. Hamad Department of Anatomy 2022 Objectives At the end of this session, students should able to • Define gametogenesis, spermatogenesis and oogenesis • Explain the mechanism of sperm and ovum formation • Describe the clinical importance of gametogenesis Gametogenesis (gamete formation) • Process involving conversion of germ cells into male and female gametes • Chromosome number is reduced by half and shape of cells is altered • Number of chromosomes is reduced during meiosis • Gametogenesis is divided into – Spermatogenesis: Male gametes production – Oogenesis: Female gametes production Meiosis Spermatogenesis • Spermatogonia are spherical to polygonal cells which contain diploid number of chromosomes • Repeated mitotic division gives rise to three types of spermatogonia – Dark Type A spermatogonia – Pale Type A spermatogonia – Type B spermatogonia • Spermatogonia will differentiate to produce primary spermatocytes • Each primary spermatocyte is diploid • Undergoes a first meiotic division to give two secondary spermatocytes • Secondary spermatocytes have the haploid number of chromosomes (22 + Y or 22 + X) • Secondary spermatocytes then divide by mitosis to give rise to spermatids • Each secondary spermatocyte gives rise to four spermatids • Young spermatids occupy deep invaginations in apical cytoplasm of cells of Sertoli • They then undergo spermiogenesis • Cells of Sertoli support and provide nutrients to the spermatids Spermiogenesis • Morphological changes that transform a spermatid into spermatozoon – discarding excess cytoplasm and growing tails • Last phase of spermatogenesis Spermiogenesis Mature sperm Transport of Spermatozoa • Despite having flagella the young spermatozoa are non-motile • Transport from seminiferous tubules to the epididymis and vas deferens is passive • Absorption of luminal fluid resulting in suction of spermatozoa into epididymis and vas deferens Seminal fluid (Semen) • Mixture of spermatozoa and the secretions from the accessory glands • Slightly alkaline in reaction and is especially rich in fructose which serves as a source of energy for the spermatozoa • Also, citric acid and hyaluronidase which facilitate the passage of spermatozoa through cervical mucus • Examination of spermatozoa in ejaculate has revealed the following facts: – Spermatozoa with Y chromosome have round and small heads, while those with X chromosomes are avoid and larger – Male spermatozoa (22+y) are about twice as numerous as female spermatozoa (22+X) – Female spermatozoa are more tolerant to acidic environments than male spermatozoa – Male spermatozoa are more speedy but have a shorter life span of not more than 24 hours – Female spermatozoa have a life span of about 72 hours. Abnormal spermiogenesis – Poorly developed acrosome hence inability to fertilize – No/poorly developed tail – Absence or decreased in mitochondria hence poor propagation of sperm • All these end up giving sperms which can not fertilize the ovum and hence infertility • Clinical Application – Azoospermia: medical condition of a man whose semen contains no sperm. Oogenesis • Development of ova from primordial germ cells or oogonia • Oogonia are diploid and have 22 pairs of autosomes and a pair of X chromosomes • Before birth oogonia undergo repeated mitotic divisions and enlarge to become primary oocytes • Primary oocytes enter first division of meiosis just before birth • For unknown reasons division is arrested at this stage until puberty • At birth there are about 200,000 follicles in each ovary • Majority of these degenerate so that only about 10,000 survive until puberty Maturation of primary oocyte • Before ovulation, primary oocyte completes first meiotic division which was started before birth • This is a reduction division resulting in a secondary oocyte with the haploid number of chromosomes • Secondary oocyte immediately undergoes a second meiotic division • But is not completed until fertilization, arrests at second metaphase. Ovulation • Follicle approaches surface of ovary and causes a stigma • Fluid-filled clefts appear in the cumulus oophorus and freeing ovum • Further increase in follicular fluid results in rupture of the stigma • Ovum is released with liquor folliculi into the peritoneal cavity • Discharged ovum usually passes into fimbriated end of uterine tube • Two main factors bring this about namely: – movement of ciliated epithelium at fimbriated end – contraction of the smooth muscle of tube • Ovum is viable for only 24 hours • If fertilization does not occur within 24 hours ovum starts to degenerate • After ovulation remaining follicle forms the corpus luteum • If fertilization does not occur it attains its greatest development at about 9th days after ovulation • Then begins to degenerate • This is the corpus leteum of menstruation • At 14 days after ovulation is completely degenerated and forms corpus albicans • If pregnancy: corpus luteum of pregnancy – produce progesterone – Thereafter its function is taken up by placenta Cyclical changes in the Female Genital System • Undergoes structural changes every month • Occur in the ovary, uterine tubes, uterus and vagina • Occur from puberty to the onset of menopause Ovarian cycles • Cyclical changes in the ovary determine the cyclic changes in the uterus • Ovarian cycles takes an average of 28 days • Divided into three phases – follicular phase – ovulatory phase – luteal phase Follicular Phase (6 – 14 days) • Commences under the influence of the follicle stimulating hormone (FSH) • Several primordial follicles develop into primary follicles and proceed to develop into graafian follicles • Developing follicles secrete mostly oestrogens and small amounts of progesterone • Rising levels of oestrogen stimulate the anterior lobe of the pituitary to produce luteinizing hormone (LH) • LH levels gradually increase, at around day 14 there is a surge of the LH secretion, leading to ovulation Functions of oestrogens 1. Development and maintenance of female secondary sexual characters 2. Prime the female so that she is attracted to the opposite sex 3. Stimulate the repair and proliferation of the endometrium before ovulation 4. Stimulate the motility of the uterus and uterine tubes 5. Stimulate growth of the uterus and its musculature during pregnancy 6. Prevent keratinisation of the vagina by increasing the glycogen content of the epithelial cells 7. Stimulate the proliferation of the duct system of the breast during pregnancy 8. Provide a feed-back mechanism which controls the outflow of gonadotrophic hormones Ovulation • Ovulation occurs at about day 14 +/- 2 • Triggered by a surge of LH production • Oocyte is released into the peritoneal cavity • Occurrence of ovulation can be estimated by – Measurement of pregnanediol in urine – Taking daily body temperature recordings Luteal Phase (14-28 days) • Lasting approximately 13 days • Coincides with formation, functioning and growth of corpus luteum • Corpus luteum produces progesterone for the following functions – Causes secretory phase of uterine cycle – Increases the tone of uterine wall If fertilization does not occur • The corpus luteum degenerates • Estrogen and progesterone levels fall and the secretory endometrium enters an ischemic phase • Menstruation occurs Uterine Cycle • Also known as the menstrual cycle • Divided into three phase – Proliferative – Secretory – Menstrual phases Proliferative Phase • Starts at the end of menstruation • Lasting approximately 9 days • Characterized by endometrial repair brought by proliferation of epithelial cells • These changes in the proliferative phase are due to oestrogens • Endometrium grows up to about 5 mm Secretory Phase • Commences after ovulation under the influence of progesterone produced by the corpus luteum • Glands become wide, tortuous and saccular • Endometrium thickens up to about 7 mm due to: – influence of progesterone and estrogen – increased fluid in the connective tissue • If pregnancy occurs the corpus luteum persists and continues to secrete progesterone • If pregnancy does not occur the corpus luteum starts to degenerate at about day 23 • Fall in progesterone levels resulting in the commencement of menstruation Menstrual Phase • Characterized by shading of blood and endometrial tissue per vaginum • Lasts about 4 to 5 days • About 50 – 60ml of blood are lost • Stratum spongiosum and part of the stratum compactum is shed during this phase • Mechanism of Menstrual phase – Vasoconstrictions of the spiral arteries – Vasodilatation causing bleeding from the damaged superficial vessels • Menstrual blood does not clot due to the presence of proteolytic enzymes Anovulatory Cycles • No ovarian follicle ruptures to release oocyte • No corpus luteum, endometrium does not progress to luteal (secretary) phase • Remains in proliferative phase until menstruation begins • Common in young girls starting to menstruate or women approaching end of their reproductive capacity