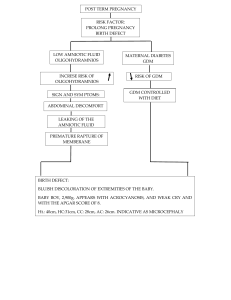
ANDREA CRISTINA IBANEZ BSN 2-12B Case Analysis: GDM 1. Pathophysiology Analysis: Gestational Diabetes Mellitus (GDM) occurs due to increased insulin resistance during pregnancy. The placenta produces hormones such as human placental lactogen, progesterone, and cortisol, which antagonize insulin action, leading to hyperglycemia. Normally, pancreatic beta cells compensate by increasing insulin secretion, but in women with GDM, this compensation is insufficient, resulting in elevated blood glucose levels. GDM affects both the mother and baby in significant ways. Mothers face a higher risk of developing pre-eclampsia, needing a cesarean section, and even developing Type 2 Diabetes later in life. Meanwhile, the baby may experience macrosomia, neonatal hypoglycemia, and long-term health issues like obesity and diabetes. 2. Risk Factor Evaluation: Obesity. Being in the obese category increases insulin resistance, making it harder for the body to regulate blood sugar levels. Maternal Age. Being over 30 increases the likelihood of GDM due to a natural decline in insulin sensitivity with age. Family History of Diabetes. A strong genetic component plays a role in GDM, and with her mother having Type 2 Diabetes, she was already predisposed to the condition. 3. Laboratory Data Interpretation: The laboratory results indicate that Mrs. Reyes' fasting blood glucose level is 105 mg/dL, which exceeds the normal limit of less than 95 mg/dL. This elevated result raises suspicion of gestational diabetes mellitus (GDM), prompting the need for an oral glucose tolerance test (OGTT) to confirm the diagnosis. The OGTT results further support the diagnosis, as three of her values exceed the established cutoff levels: - - 1-hour OGTT: 185 mg/dL 2-hour OGTT: 165 mg/dL - 3-hour OGTT: 145 mg/dL Additionally, her HbA1c level is recorded at 5.9%, which falls above the normal range of 4% to 5.6%, indicating impaired glucose regulation. These findings confirm the diagnosis of GDM, highlighting the need for appropriate management to prevent complications for both the mother and the baby. 4. Clinical Management Plan: ○ Nursing Diagnosis: Imbalanced Nutrition: More than Body Requirements related to obesity as evidenced by BMI of 33 ○ Goals and Expected Outcomes: - The patient will demonstrate an understanding of proper nutrition and its role in managing GDM. - The patient will adopt healthier eating habits and engage in regular physical activity to support weight management. - The patient will maintain blood glucose levels within the recommended range throughout pregnancy. ○ Nursing Interventions with Rationales 1. Assess the patient’s current dietary habits, food preferences, and eating patterns. Understanding the patient’s usual intake helps identify unhealthy habits and provides a basis for individualized dietary recommendations. 2. Educate the patient on proper portion sizes and balanced nutrition. A well-balanced diet supports blood glucose control and prevents excessive weight gain, reducing risks associated with GDM. 3. Encourage the patient to engage in moderate physical activity, such as walking for at least 30 minutes daily. Regular exercise improves insulin sensitivity and helps with weight control. 4. Encourage physical activity such as walking for at least 30 minutes daily. This Improves insulin sensitivity and helps with weight control. 5. Monitor blood glucose levels regularly and provide guidance on self-monitoring techniques. Frequent monitoring allows early detection of glycemic imbalances, helping the patient make necessary dietary and lifestyle adjustments. 5. Patient Education and Self-Management Strategies: To help Mrs. Reyes manage her GDM, patient education should focus on practical lifestyle changes that fit into her daily routine. 1. Dietary Changes: - Balance carbohydrate intake by choosing whole grains and fiber-rich foods. - - Avoid sugary and processed foods that can spike blood sugar levels. Incorporate lean proteins and healthy fats to promote satiety and stable glucose levels. - Eat smaller, more frequent meals to prevent blood sugar fluctuations. 2. Exercise: - Engage in moderate-intensity activities such as walking for at least 30 minutes a day. - Perform light resistance exercises to improve insulin sensitivity and muscle glucose uptake. 3. Glucose Monitoring: - Check blood sugar levels regularly as advised by the healthcare provider. - Keep a log of readings to identify patterns and adjust lifestyle choices accordingly. 4. Pharmacological Interventions: - If necessary, take prescribed medications such as insulin or metformin as directed. - Understand the proper administration and potential side effects of any prescribed treatments. 6. Potential Complications and Prevention: Poorly managed GDM can lead to serious complications for both mother and baby. For the mother, there’s an increased risk of hypertension, pre-eclampsia, and developing Type 2 Diabetes after pregnancy. For the baby, complications include macrosomia, which increases the chances of birth trauma, as well as neonatal hypoglycemia and respiratory distress syndrome. To prevent these, it is best to emphasize the importance of strict glycemic control through a well-balanced diet, regular physical activity, and, if needed, medication. Additionally, regular prenatal check-ups and fetal monitoring can help identify potential complications early, ensuring timely intervention to optimize maternal and fetal health outcomes. 7. Ethical and Cultural Considerations: When caring for Mrs. Reyes, it is important to respect her autonomy and cultural background. Healthcare providers should involve her in decision-making, ensuring she understands all her options regarding treatment, diet, and lifestyle changes. If she has preferences, the healthcare team should work with her to find ways to incorporate them while maintaining proper nutrition. Additionally, all health education should be delivered in a way that is easy for her to understand, avoiding medical jargon that may be overwhelming. And building trust and providing support, healthcare providers can help her feel confident in managing her condition, leading to better health outcomes for both her and her baby. Reflection Questions: 1. What were the most complex aspects of analyzing this case? The most challenging part of analyzing this case was understanding the pathophysiology of GDM. Tracing its causes and effects required deeper research, and I encountered medical terms that were unfamiliar, making it harder to fully grasp the condition. 2. How can this activity enhance your readiness for real-life clinical practice? This activity helped me understand GDM better, including how to assess, educate, and care for pregnant patients with the condition. It also prepared me to provide proper interventions and patient education to improve both the mother and the baby, which I can apply when I am assigned to a real-life clinical setting. 3. What additional information or resources would aid in managing this patient effectively? Support from a dietitian or diabetes educator, educational materials will help Mrs. Reyes manage her condition effectively. Additionally, guidelines from accredited organizations like the American Diabetes Association (ADA) would provide helpful recommendations. Evaluation Criteria: ● ● ● ● Depth and accuracy of case analysis (40%) Application of critical thinking and clinical reasoning (30%) Organization and clarity of responses (20%) Presentation and participation (10%)